|
 |
Back to 2015 Annual Meeting Program
Ex-Vivo Lymphadenectomy During Gastrectomy for Adenocarcinoma Optimizes Lymph Node Yield
Cheguevara Afaneh*1, 2, ADAM Levy1, 2, Luke V. Selby2, Geoffrey Ku3, Sam S. Yoon2, Laura H. Tang4, Daniel G. Coit2, Vivian E. Strong2, 1
1Surgery, NY Presbyterian Hospital, New York, NY; 2Surgery, Memorial Sloan Kettering Cancer Center, New York, NY; 3Medicine, Memorial Sloan Kettering Cancer Center, New York, NY; 4Pathology, Memorial Sloan Kettering Cancer Center, New York, NY
Introduction: Variability in surgical and pathological techniques in Western centers may lead to inconsistency in lymph node staging in patients with gastric adenocarcinoma. We hypothesize that ex-vivo lymphadenectomy after gastrectomy for adenocarcinoma increases lymph node yield.
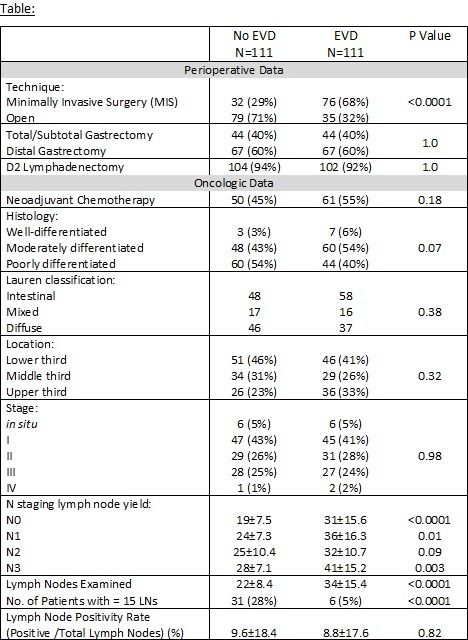
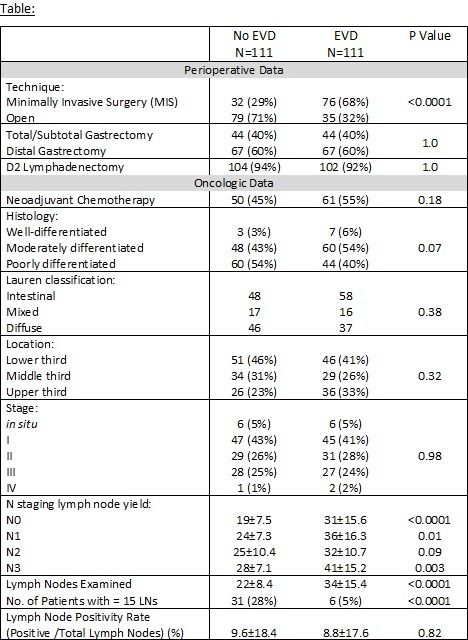
Methods: We retrospectively reviewed a series of 222 patients who underwent gastrectomy for adenocarcinoma with curative intent between November 2010 and June 2014. In August of 2012, we began performing ex-vivo dissection of nodes in our surgical specimens (EVD group), as opposed to submitting specimens en-bloc with the lymph node basins attached to the specimen (No EVD group). We compared these two methods of lymph node submission on lymph node yield.
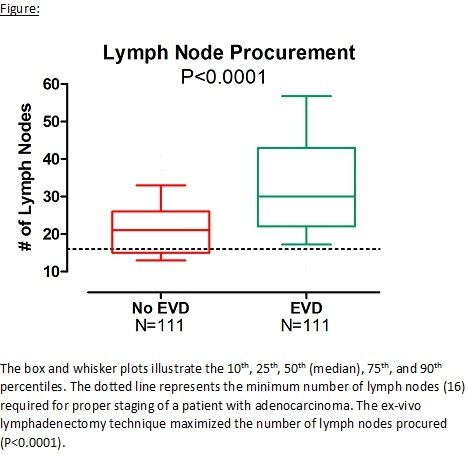
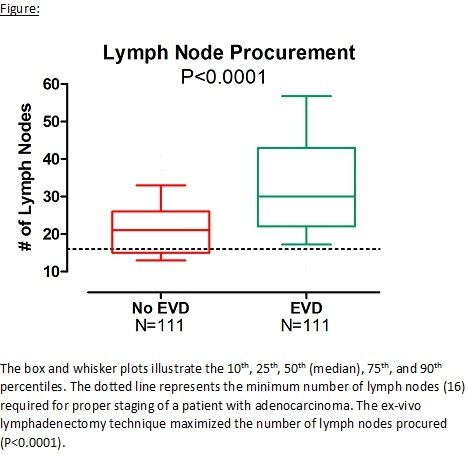
Results: There were no significant differences between the No EVD and EVD groups with respect to mean [±SD] age (62±13.6 v. 61±15.6 years, respectively; P=0.97), gender (Male: 53% v. 54%, respectively; P=1.0), or body mass index (26.9±5.3 v. 26.6±4.8 kg/m2, respectively; P=0.81). More patients underwent open gastrectomy in the No EVD group compared to the EVD group (71% vs. 32%, respectively; P<0.0001). There were no significant differences in the distribution of total/subtotal gastrectomies and D2 lymphadenectomies (Table). Use of neoadjuvant therapy, tumor histology, location, and final pathologic staging were similar between the two groups. The median number of lymph nodes procured was significantly higher in the EVD group compared to the No EVD group (30 vs 21 lymph nodes, respectively; P<0.0001). Moreover, 28% of the No EVD group were not adequately staged (defined by ≤ 15 nodes), compared to 5% of the EVD group (P<0.0001). Patients undergoing open gastrectomy had a significantly lower mean number of lymph nodes procured compared to minimally invasive gastrectomies (26±14 vs. 30±14, respectively; P=0.02). However, there was no difference in lymph node yield in patients undergoing EVD based on surgical technique (Open: 35±19 vs. MIS: 33±14; P=0.89). Lymph node yield was significantly higher in the EVD group compared to the No EVD group for N0 (P<0.0001), N1 (P=0.01), and N3 (P=0.003) disease (Table).
Conclusions: Ex-vivo lymphadenectomy may be a useful tool to maximize lymph node yield. This may be an important adjunct to staging patients in situations where insufficient nodes are routinely retrieved and examined. Further studies and longer follow-up are necessary to assess any impact this may have on stage migration and improve patient selection for postoperative adjuvant treatment.
Back to 2015 Annual Meeting Program
|