Back to 2015 Annual Meeting Program
Defining the Impact of Surgical Approach on Perioperative Outcomes for Patients With Gastric Cardia Malignancy
Ryan W. Day*, Brian Badgwell, Keith F. Fournier, Paul F. Mansfield, Thomas Aloia
Surgical Oncology, MD Anderson, Houston, TX
Background: Although the American College of Surgeons National Surgical Quality Improvement Program (ACS-NSQIP) database is positioned to assess outcomes for patients with proximal gastric cancer, previous analyses focused on either gastrectomy for any-site gastric tumor or esophagectomy for any-site esophageal tumor. In contrast to these whole organ-based analyses that were not specific to gastric cancer, the purpose of the current study was to compare outcomes associated with three common operative approaches by focusing only on a homogeneous cohort of patients with gastric cardia malignancy.
Methods: The ACS-NSQIP Participant Use File was searched to identify all patients with gastric cardia malignancy (ICD-9 151.00) who underwent total gastrectomy (TG, CPTs 43620, 43621 and 43622), transhiatal esophagectomy (THE, CPT 43107) or thoraco-abdominal esophagectomy (TAE, CPTs 43112 and 43117) between 2005 and 2012. Demographic, perioperative risk factors and outcomes including rates of 30-day major morbidity, overall morbidity and mortality were analyzed with standard statistical measures. Major morbidity was defined as organ space infection, pneumonia, unplanned intubation, pulmonary embolism, ventilator requirements >48 hours, progressive renal insufficiency, acute renal failure, cerebrovascular accident, coma, cardiac arrest, myocardial infarction, deep venous thrombosis, sepsis, septic shock, and return to the operating room.
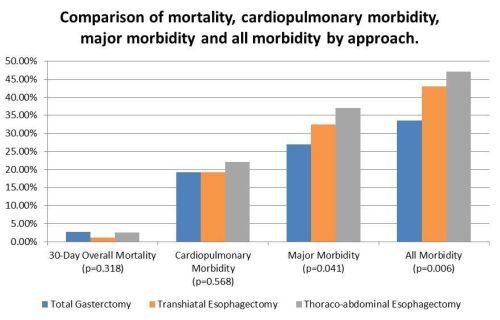
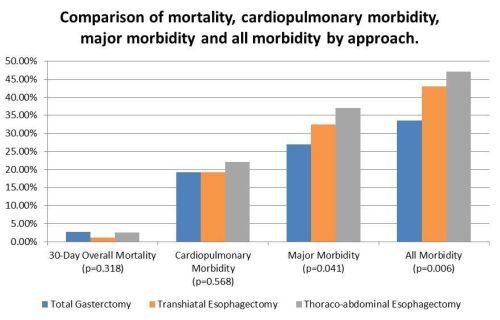
Results: Demographic features of the 977 identified study patients included 805 males (82.4%), with median age of 65 (range: 20-89), median BMI 26.9 (range: 15.5-52.6) and mean ASA was 2.84. Resections included TG: 182 (18.6%), THE: 281 (28.8%), and TAE: 514 (52.6%). Despite TAE patients being younger, this group had higher proportion of ASA class III/IV and longer operative times (Table 1). There was no significant difference in 30-day mortality between the groups, however overall morbidity and major morbidity were significantly higher in the group undergoing TAE (Figure 1). On multivariate analysis, independent predictors of major morbidity were ASA class III/IV, alcohol use, COPD, previous coronary surgery, operation in the previous 30 days and operative approach (all p<0.05). Risk factors independently associated with mortality were diabetes, COPD, prior myocardial infarction, renal failure and operation in the previous 30 days (all p<0.05).
Conclusion: For patients with proximal gastric cancer, the three most common operative approaches were associated with clinically-significant rates of major morbidity. Although abdominal approaches were associated with decreased morbidity, they were utilized less frequently. These data suggest that approach-associated morbidity should be considered along with tumor location and extent when choosing a technique for oncologic resection of gastric cardia malignancy.
Univariate analysis of outcome measures in patients undergoing total gastrectomy, transhiatal esophagectomy and thoraco-abdominal esophagectomy
| Factor | Total Gastrectomy (n=182) | Transhiatal Esophagectomy (n=281) | Thoraco-abdominal Esophagectomy (n=514) | p-value |
| Operative Time† | 315.26 +/- 123.31 | 297.66 +/- 106.38 | 390.01 +/- 124.81 | <0.001 |
| SSI* | 10 (5.5%) | 27 (9.6%) | 39 (7.6%) | 0.264 |
| Deep SSI* | 5 (2.7%) | 11 (3.9%) | 5 (1.0%) | 0.016 |
| Organ Space Infection* | 17 (9.3%) | 18 (6.4%) | 33 (6.4%) | 0.376 |
| Dehiscence** | 3 (1.6%) | 7 (2.5%) | 5 (1.0%) | 0.224 |
| Pneumonia* | 21 (11.5%) | 33 (11.7%) | 71 (13.8%) | 0.602 |
| Reintubation* | 9 (4.9%) | 28 (10.0%) | 61 (11.9%) | 0.028 |
| Pulmonary Embolism** | 4 (2.2%) | 5 (1.8%) | 13 (2.5%) | 0.807 |
| Ventilator >48 Hours* | 20 (11.0%) | 24 (8.5%) | 63 (12.3%) | 0.276 |
| Progressive Renal Insufficiency** | 2 (1.1%) | 0 (0.0%) | 7 (1.4%) | 0.094 |
| Acute Renal Failure** | 1 (0.5%) | 3 (1.1%) | 10 (1.9%) | 0.446 |
| UTI* | 6 (3.3%) | 9 (3.2%) | 16 (3.1%) | 0.992 |
| Stroke** | 4 (2.1%) | 0 (0.0%) | 0 (0.0%) | 0.001 |
| Coma** | 1 (0.5%) | 0 (0.0%) | 1 (0.2%) | 0.421 |
| Cardiac Arrest** | 2 (1.1%) | 3 (1.4%) | 11 (2.1%) | 0.677 |
| MI** | 0 (0.0%) | 1 (0.4%) | 10 (1.9%) | 0.048 |
| Post-op Transfusion* | 17 (9.3%) | 26 (9.3%) | 70 (13.6%) | 0.247 |
| DVT* | 5 (2.7%) | 10 (3.6%) | 26 (5.1%) | 0.335 |
| Sepsis* | 20 (11.0%) | 28 (10.0%) | 57 (11.1%) | 0.881 |
| Septic Shock* | 11 (6.0%) | 16 (5.7%) | 40 (7.8%) | 0.479 |
| Return to OR* | 19 (10.4%) | 30 (10.7%) | 71 (13.8%) | 0.307 |
| 30 Day Mortality** | 5 (2.7%) | 3 (1.1%) | 13 (2.5%) | 0.318 |
| CP Morbidity* | 35 (19.2%) | 54 (19.2%) | 113 (22.0%) | 0.568 |
| Any Morbidity* | 61 (33.5%) | 121 (43.1%) | 242 (47.1%) | 0.006 |
| Major Morbidity* | 49 (26.9%) | 91 (32.4%) | 190 (37.0%) | 0.041 |
| Hospital LOS† | 14.36 +/- 11.64 | 13.10 +/- 10.81 | 13.96 +/- 13.96 | 0.100 |
SSI=Surgical Site Infection, UTI=Urinary Tract Infection, MI=Myocardial Infarction, DVT=Deep Vein Thrombosis, OR=Operating Room, CP=Cardiopulmonary, LOS=Length of Stay,*=Chi-Squared, **=Fisher's Exact Test, †=Kruskal-Wallis Test
Back to 2015 Annual Meeting Program