|
Back to 2015 Annual Meeting Program
Impact of Sarcopenia on Short- and Long-Term Outcomes in Patients Undergoing Curative Intent Resection for Pancreatic Adenocarcinoma: a New Tool
Neda Amini*1, Rohan Gupta1, Georgios a. Margonis1, Yuhree Kim1, Gaya Spolverato1, Neda Rezaee1, Matthew J. Weiss1, Christopher L. Wolfgang1, Martin a. Makary1, Ihab R. Kamel2, Timothy M. Pawlik1
1Department of Surgery, The Johns Hopkins University School of Medicine, Baltimore, MD; 2Department of Radiology, The Johns Hopkins University School of Medicine, Baltimore, MD
Background: Sarcopenia, defined as loss of muscle mass, may be a more objective means to determine peri-operative performance status. Traditionally, sarcopenia has exclusively been characterized using total psoas area (TPA). Defining sarcopenia using only a single axial cross-sectional image may, however, be inadequate. We sought to evaluate total psoas volume (TPV) as a new tool to define sarcopenia and compared TPV with traditional TPA.
Method: Sarcopenia was assessed in 763 patients who underwent pancreatectomy for pancreatic adenocarcinoma between 1996-2014. Sarcopenia was defined as the TPA and TPV in the lowest sex-specific quartile. The impact of TPA and TPV sarcopenia on overall morbidity and mortality was assessed using multivariable analysis.
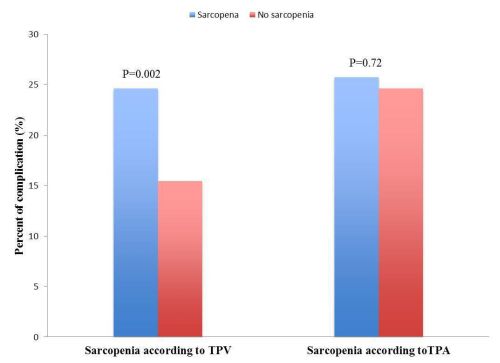
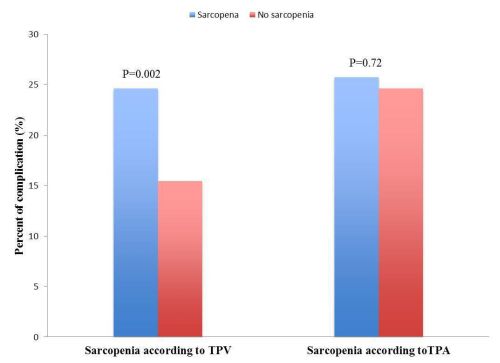
Result: Median patient age was 67 years and 54.8% (n= 418) was male. Median TPA and TPV were both lower in women (506.3mm2/m2 and 22.4 cm3/m2, respectively) versus men (685.1mm2/m2 and 33.0 cm3/m2, respectively)(both P<0.001). 192 (25.1%) patients had sarcopenia by TPA, while 152 patients (19.9%) had sarcopenia according to TPV. Post-operatively, 369 (48.4%) patients had a complication. While TPA-sarcopenia was not associated with the risk of morbidity (OR=1.06; P= 0.72), sarcopenia defined by TPV was associated with a higher odds of complications (OR= 1.79; P= 0.002). In fact, patients with sarcopenia according to TPV had a higher risk of a major complication (Clavien grade ≥3)(22.4% vs. 15.1%; P= 0.03) and a longer length-of-stay (10 days vs. 8 days; P=0.002). On multivariable analysis, TPV-sarcopenia remained independently associated with an increase risk of post-operative complication (OR= 1.69; P= 0.006). In addition, after controlling for competing risk factors, sarcopenia defined by TPV was associated with a higher odds of long-term death (HR=1.46; P= 0.006).
Conclusion: The use of TPV to define sarcopenia was associated with both short- and long-term outcomes following resection of pancreatic cancer. Assessment of the entire volume of the psoas muscle (TPV) may be a better means to define sarcopenia rather than a single axial image (TPA).
Back to 2015 Annual Meeting Program
|