|
Back to 2015 Annual Meeting Program
Both Pre-Transplant and Early Post-Transplant Anti-Reflux Surgery Prevent Development of Early Allograft Injury After Lung Transplantation
Wai-KIT Lo*1, 2, Jon Wee3, Piero Marco Fisichella4, Walter W. Chan1
1Division of Gastroenterology, Hepatology and Endoscopy, Brigham and Women's Hospital, Boston, MA; 2Gastroenterology, VA Boston Healthcare System, Boston, MA; 3Division of Thoracic Surgery, Brigham and Women's Hospital, Boston, MA; 4Surgery, VA Boston Healthcare System, Boston, MA
Background: Anti-reflux surgery (ARS) has been associated with improved lung transplant outcomes. Pre-transplant ARS has been shown in small studies to improve pulmonary function among transplant candidates with gastroesophgeal reflux disease (GERD). Although early post-transplant ARS has been more effective than later ARS in reducing chronic rejection, the optimal timing of ARS in transplant recipients remains unclear.
Aim: To evaluate the time to early allograft injury among lung transplantation recipients by timing of ARS before and after transplantation.
Methods: This was a retrospective cohort study of lung transplant patients undergoing ARS before or after transplantation at a tertiary care center since 2007, with at least one year follow-up. Early allograft injury was defined clinically and histologically as acute rejection or lymphocytic bronchiolitis, occurring within the first year after transplantation. In accordance with prior studies, the cutoff between early and late post-transplant ARS was 6 months. Time-to-event analysis using the Cox proportional hazards model was applied to assess the relationship between timing of surgery and early allograft injury. Subjects not meeting this outcome were censored at one year in the time-to-event analysis. Fisher's exact test for binary variables and student's t-test for continuous variables were performed to assess for differences between surgical timing groups.
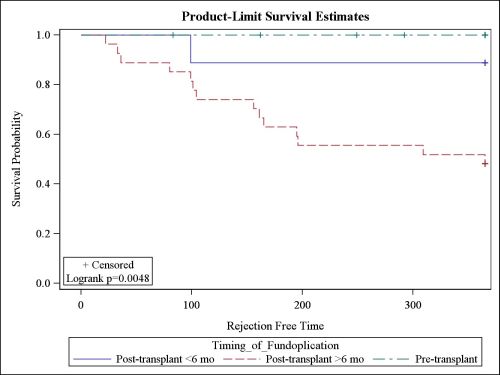
Results: 48 subjects (60% men, mean age: 55, average follow-up: 3.5 years) met inclusion criteria for the study. Patient demographics, pre-transplant cardiopulmonary function, BMI, CMV status, and PPI exposure were similar between groups. Kaplan-Meier analysis (Figure 1) demonstrated significantly increased early allograft injury in late post-transplant ARS patients compared with both pre-transplant (log-rank p=0.007) and early post-transplant (log-rank p=0.05) patients, as well as a significant trend across groups (log-rank p=0.005). No significant difference between pre-transplant and early post-transplant groups was noted (Table 1). Complications were rare and identified in 1 pre-transplant fundoplication patient with recurrent symptoms requiring re-operation, and in 3 late post-transplant ARS patients: 2 with recurrent symptoms and regurgitation requiring re-operation, and 1 with aspiration pneumonia resulting in death. No early post-transplant ARS patients experienced complications.
Conclusion: Late post-lung transplant ARS resulted in increased risk of early allograft injury compared to pre-transplant and early post-transplant ARS. Both pre-transplant and early post-transplant ARS appear equally safe and effective in improving lung transplant outcomes. These findings support consideration of anti-reflux measures before and soon after transplantation to minimize the impact of reflux on allograft injury and longer term outcomes.
| Fundoplication Timing and Early Allograft Injury | Kaplan-Meier Log-rank P-value | | Late Post-transplant vs. Pre-transplant | 0.007* | | Late Post-transplant vs. Early Post-transplant | 0.05* | | Early Post-transplant vs. Pre-transplant | 0.25 |
Table 1. Kaplan-Meier Log-rank P-value demonstrating increased early allograft injury associated with late post-transplant surgical fundoplication compared to early post-transplant or pre-transplant surgical fundoplication. * = statistically significant 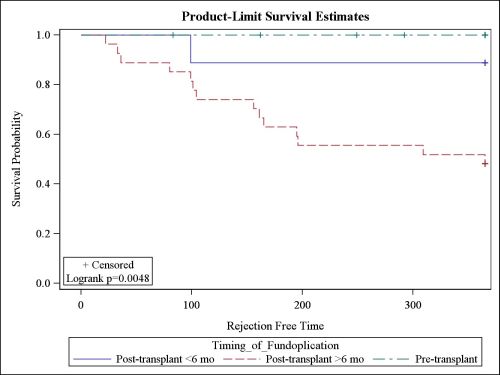 Figure 1. Kaplan-Meier Analysis of time to early allograft injury by timing of fundoplication. Late post-transplant surgical fundoplication was associated with increased early allograft injury compared to early post-transplant and pre-transplant surgical fundoplication.
Back to 2015 Annual Meeting Program
|