|
 |
Back to 2015 Annual Meeting Program
Trends in Receipt and Timing of Multimodality Therapy in Early Stage Pancreatic Cancer
Francesca Dimou*1, 2, Helmneh Sineshaw4, Abhishek Parmar3, Nina Tamirisa1, 3, Daniel Jupiter1, Ahmedin Jemal4, Taylor S. Riall1
1University of Texas Medical Branch, Houston, TX; 2University of South Florida, Tampa, FL; 3University of San Francisco, East Bay, Oakland, CA; 4American Cancer Society, Atlanta, GA
INTRODUCTION: For patients with locoregional pancreatic cancer multimodality therapy (MMT) with surgical resection and chemotherapy is the standard of care. The objective of this study was to evaluate contemporary treatment patterns and time trends in receipt of multimodality therapy and timing of chemotherapy relative to surgery in patients undergoing MMT for locoregional pancreatic cancer.
METHODS: We used the National Cancer Data Base (NCDB) to identify patients >18 years of age with stage I and II pancreatic adenocarcinoma (excluding T3 tumors). Treatment groups were defined as no treatment, surgical resection only, chemotherapy only, or MMT with chemotherapy (neoadjuvant or adjuvant) and surgery. Trends in receipt of surgery, chemotherapy, or MMT were compared. Kaplan-Meier curves were used to evaluate survival based on treatment modality.
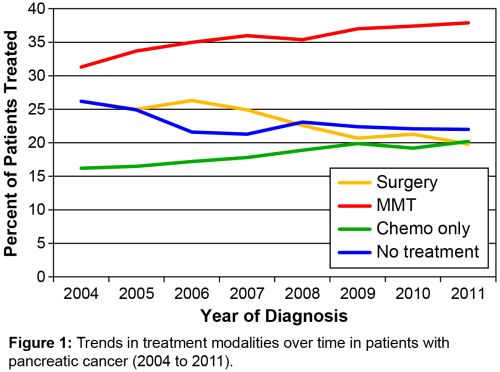
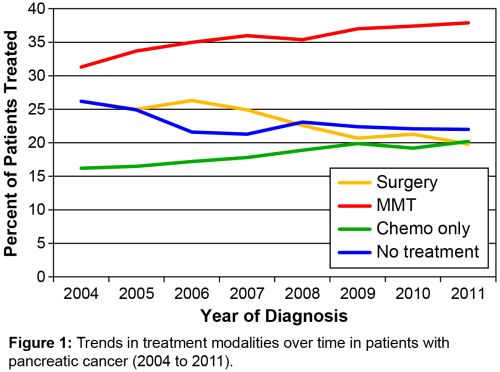
RESULTS: A total of 39,441 patients were identified. The mean age of the cohort was 68.1+11.6 years. 73.6% were white; 40.1% were treated at a community center/cancer program. 22.8% of patients received no treatment. Patients ≥76 years of age had lower receipt of treatment compared with those aged 15-55 years (54.8% vs. 90.6%) (p<0.0001). Community cancer programs (68.8%) and community cancer centers (72.1%) were less likely to treat patients than NCI-designated Cancer Cancers (85.2%, p<0.0001). Of 30,445 treated patients, 29.8% underwent only surgical resection, 23.9% received chemotherapy only, and 46.3% received MMT. Receipt of MMT increased from 31.3% of the overall cohort in 2004 to 37.9% in 2011 (p<0.0001)(Figure 1). Chemotherapy was delivered in the neoadjuvant setting in 4.5% of patients receiving MMT in 2004 and 16.7% in 2011 (p<0.0001). Neoadjuvant therapy comprised a greater proportion of MMT at NCI cancer centers (16.8%) compared to community cancer programs (5.6%) and comprehensive community cancer centers (7.9%). In patients who underwent surgery at the initial treatment modality (N=21,633), 58.1% received adjuvant therapy; adjuvant therapy decreased from 68.4% of patients 18-55 to 38.3% of patients >76 years who underwent surgery first. Regardless of the timing of chemotherapy, patients had improved survival if they received MMT; 2-year survival was 46.9% for MMT (46.5% adjuvant vs. 49.5% neoadjuvant).
CONCLUSION: In this contemporary cohort, receipt of MMT increased over time, but remained underutilized. Older patients and patients treated in community programs were more likely to be untreated. Despite multiple single-institution reports, MMT is still most commonly delivered in the adjuvant setting, though the proportion of MMT delivered in the neoadjuvant setting is increasing. When surgery is the initial treatment modality, a third of patients do not go on to receive adjuvant therapy with the greatest disparity occurring in older patients.
Back to 2015 Annual Meeting Program
|