|
Back to 2015 Annual Meeting Program
To Capture Complication-Related Readmission After Pancreatectomy "90-Days From Surgery" Is Superior to "30-Days From Discharge"
Yoshihiro Mise*, Matthew H. Katz, Ryan W. Day, Kristoffer W. Brudvik, Lilian Schwarz, Claudius Conrad, Jean-Nicolas Vauthey, Jeffrey E. Lee, Jason B. Fleming, Thomas Aloia
Surgical Oncology, MD Anderson, Houston, TX
Background: Although hospital readmission after pancreatectomy is an important measure of the quality of surgical treatment, it can be difficult to isolate readmissions related to surgical complications from those related to medical, oncologic or other issues. Previous studies have defined the readmission interval as either "30-Days from Discharge" or "90-Days from Surgery". The objective of this study was to determine which of these definitions best captures readmissions that occur as a direct result of surgical complications after pancreatectomy.
Methods: A prospectively maintained database at a high volume HPB surgery center was queried to identify individuals who underwent pancreatectomy between 2000 and 2012. All cases of readmission in the 365 days following the initial operation were identified, indexed by cause, and stratified according to a standard grading scale. Unplanned disease-related readmissions were defined as those caused by symptoms of radiologically or pathologically confirmed disease progression. All other unplanned readmissions were defined as complication-related readmissions and categorized. The data was analyzed at 30-days after discharge and 90-days after operation in order to compare the capture rates of complication-related readmissions. Multivariable analysis assessed risk-factors for readmission at each time point.
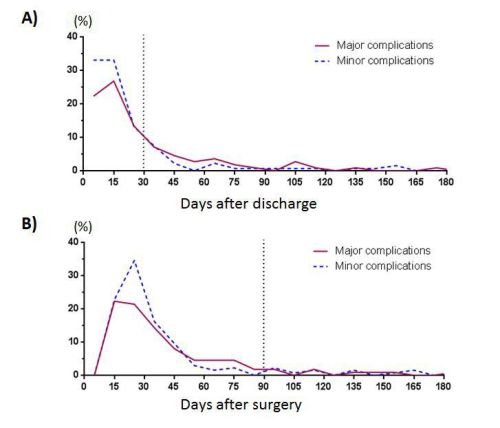
Results: During the study period, 1,123 patients were discharged from hospitalization after pancreatectomy. Complication-related readmissions occurred in 248 (22%) individuals while readmissions related to disease progression occurred in 25 (2%) individuals. For patients with a complication-related readmission, 93 (37.5%) readmissions were associated with a major adverse event requiring intervention or ICU admission. The "30-Days from Discharge" definition encompassed 184 complication-related readmissions and 1 disease-related readmission (sensitivity: 0.74, specificity: 0.96). In contrast, the "90-Days from Surgery" definition captured 215 complication-related readmissions and 1 disease-related readmission (sensitivity 0.87, specificity 0.96). The "30-Days from Discharge" definition captured only 66 (sensitivity 0.71) major surgical complications, while the "90-Days from Surgery" definition captured 84 major surgical complications (sensitivity 0.90). For the subset of readmissions uniquely captured by the "90-Days from Surgery" definition, major complication was the only independent risk factor for readmission (p=0.02, HR: 3.94, 95% CI 1.44-12.22).
Conclusions: The "90-Days from Pancreatectomy" readmission definition more precisely captures readmissions directly related to surgical morbidity, particularly those associated with major complications. These data indicate that this readmission definition should routinely be used after pancreatectomy.
Clinicopathological features of pancreatectomy readmissions
| Factor | 30-Days from Discharge (n=184) | 90-Days from Surgery not Captured by 30-Day from Discharge (n=31) | Univariate p-value | Multivariate p-value | | Demographics | | Age >65 | 83 (45%) | 9 (29%) | 0.09 | 0.13 | | Male | 100 (54%) | 19 (61%) | 0.47 | | | ASA score >2 | 115 (79%) | 13 (62%) | 0.09 | 0.18 | | Surgery and Hospitalization | | PD | 132 (72%) | 22 (71%) | 0.93 | | | DP | 45 (24%) | 7 (23%) | 0.82 | | | EBL (cc)** | 700 (50-9550) | 700 (150-4700) | 0.86 | | | IH LOS (days)** | 11 (5-67) | 10 (6-50) | 0.24 | | | IH Complication | 16 (9%) | 4 (13%) | 0.46 | | | Causes of Readmission | | Fluid Collection | 54 (29%) | 11 (35%) | 0.49 | | | Hemorrhage* | 5 (3%) | 2 (6%) | 0.28 | | | Biliary* | 3 (2%) | 2 (6%) | 0.09 | 0.27 | | Ileus* | 2 (1%) | 2 (6%) | 0.04 | 0.39 | | Major Direct Complications | 66 (36%) | 18 (58%) | 0.02 | 0.02 |
ASA= American Society of Anesthesiologists, PD = Pancreaticoduodenectomy DP = Distal Pancreatectomy, EBL = Estimated Blood Loss, IH = Index hospitalization, LOS = Length of Stay, *=Fisher's Exact Test, **=Mann-Whitney U Test, All others Chi-Squared 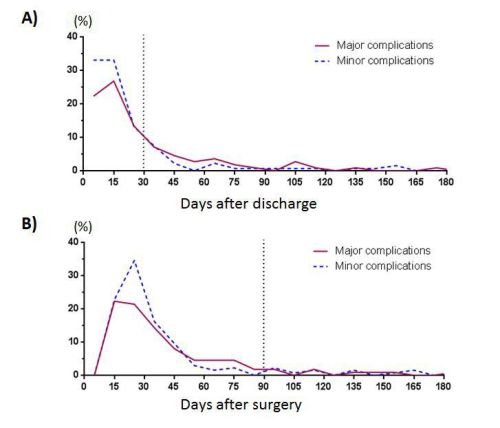
Back to 2015 Annual Meeting Program
|