|
 |
Back to 2015 Annual Meeting Program
Watch and Wait? - Elevated Pretreatment CEA Is Associated With Decreased Pathological Complete Response in Rectal Cancer
Christian P. Probst*1, Adan Z. Becerra1, Mohamedtaki a. Tejani2, Christopher T. Aquina1, Bradley J. Hensley1, Maynor G. GonzáLez1, Katia Noyes1, John R. Monson1, Fergal Fleming1
1Surgical Health Outcomes & Research Enterprise, Department of Surgery, University of Rochester Medical Center, Rochester, NY; 2Department of Medicine - Hematology/Oncology Division, University of Rochester Medical Center, Rochester, NY
Introduction: Between 10% and 30% of rectal cancer patients experience pathological complete response (pCR) after neoadjuvant treatment. In parallel with this, there is increasing interest in the concept of adopting a ‘watch and wait' policy following neoadjuvant chemoradiation in patients who manifest endoscopic and radiographic tumor regression. However, physiological factors predicting which patients will experience tumor response and ultimately pCR after clinical complete response are largely unknown. Prior studies have suggested an association between elevated pretreatment carcinoembryonic antigen (CEA) levels and lower rate of pCR, but have been limited by small sample sizes. In contrast, this study sought to examine the relationship between pre-treatment CEA and pCR in a large validated, population-based cohort.
Methods: Patients with clinical stage II and III rectal cancer who underwent neoadjuvant chemoradiation and surgical resection with curative intent were selected from the 2006-2011 National Cancer Data Base. CEA was defined as normal, borderline and elevated based on the standards of each facility laboratory. Bivariate analysis was used to examine pCR rates across patient, tumor, and facility characteristics. Separate logistic regression models were used to estimate the odds of pCR, pathological tumor regression and tumor downsizing associated with normal, borderline, and elevated CEA levels after controlling for pertinent covariates.
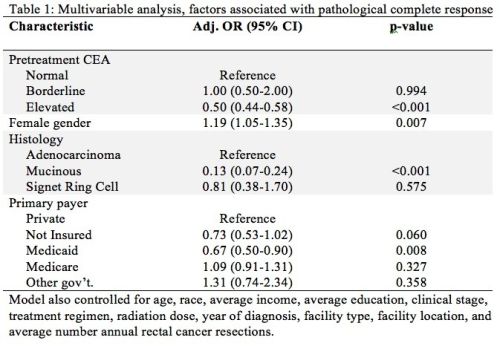
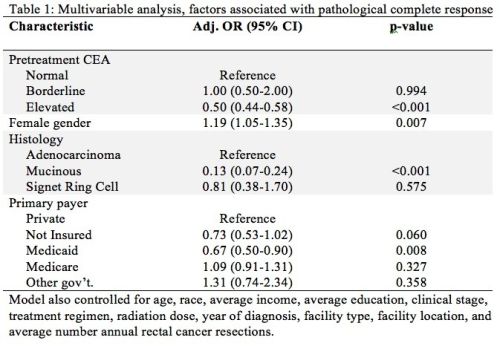
Results: Of 11,029 patients meeting inclusion criteria, 44% had elevated CEA and 12% experienced pCR. On bivariate analysis, elevated CEA was associated with decreased odds of pCR (OR=0.47, 95%CI=0.42-0.54, p<0.001). After adjusting for covariates, patients with an elevated CEA had a 50% decrease in the odds of pCR as compared to those with normal CEA (OR=0.50, 95%CI=0.44-0.58, p<0.001). Additionally, elevated CEA was associated with reduced pathological tumor regression (OR=0.63, 95%CI=0.54-0.73, p<0.001) and reduced tumor downsizing (OR=0.55, 95%CI=0.51-0.60, p<0.001). There was no observed effect of borderline CEA on pCR (Table 1), tumor regression or tumor downsizing.
Conclusion: Rectal cancer patients with an elevated pretreatment CEA are less likely to experience pCR, pathological tumor regression and tumor downsizing after neoadjuvant treatment. This may reflect unfavorable tumor biology or decreased responsiveness to treatment. These patients are very unlikely to achieve a significant tumor response following neoadjuvant therapy and are probably not suitable for a watch and wait strategy. These patients would most likely benefit from prompt surgical resection and expeditious delivery of adjuvant therapy rather than an extended duration between completion of neoadjuvant treatment and surgery as the likelihood of a significant tumor response is quite low.
Back to 2015 Annual Meeting Program
|