|
Back to 2015 Annual Meeting Program
Survival After Resection of Gastrointestinal Stromal Tumor and Sarcoma Liver Metastases: a Single-Center Experience of 146 Patients
Kristoffer W. Brudvik*, Sameer H. Patel, Thomas Aloia, Claudius Conrad, Kelia E. Torres, Christina L. Roland, Kelly K. Hunt, Janice N. Cormier, Barry W. Feig, Jean-Nicolas Vauthey
Surgical Oncology, The University of Texas, MD Anderson Cancer Center, Houston, TX
Background: In the current literature, gastrointestinal stromal tumors (GIST), leiomyosarcomas (LMS), and other sarcomas (SRC) have often been assessed together when reporting outcomes after resection of their liver metastases (LM). The aim of the present study was to separately investigate outcomes according to each pathological entity in a large patient series.
Method: The institutional liver database was used to identify patients who underwent liver resection from 1998 through 2013. Histopathological, clinical and survival data were updated and analyzed.
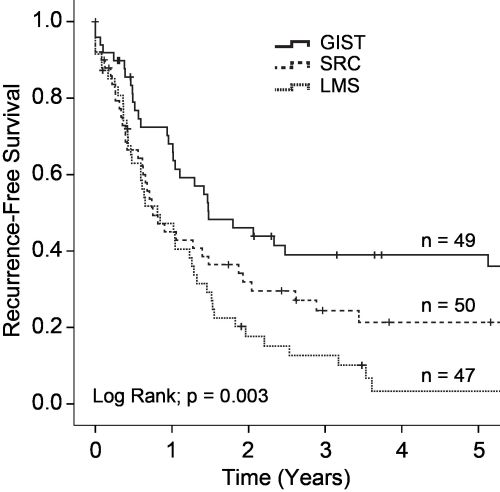
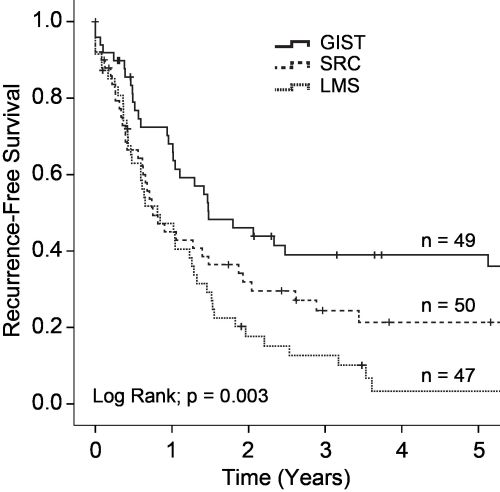
Results: A total of 146 patients underwent resection of LM: GIST, n = 49; LMS, n = 47; SRC, n = 50. The 5-year overall survival (OS) were 55.2%, 48.4%, and 44.9% and the 10-year OS were 52.5%, 9.2%, and 23.0% in patients with GIST, LMS, and SRC, respectively. GIST were associated with improved 5-year recurrence-free survival (RFS; 35.7%; p = 0.003) compared to SRC (3.4%) and LMS (21.4%; Figure). The rate of liver recurrence was similar (34.0%-40.8%) for the three pathological entities. Lung recurrence was more common in patients with LMS (36.2%; p < 0.0001) than in patients with SRC (12.0%) and GIST (2.0%). Patients resected for GIST LM had improved 5-year RFS if they received perioperative treatment with imatinib (imatinib: 47.1%; resection-only: 9.5%; p = 0.013), but not 5-year OS (imatinib: 57.5%; resection-only: 50.0%; p = 0.950). Patients resected for LMS LM had the same 5-year RFS regardless of the location of the primary (intraabdominal: 14.5%; other location: 0%; p = 0.182).
Conclusion: LM from GIST, LMS, and SRC should be assessed separately as the survival and recurrence patterns are different. This is especially important for GIST since the introduction of targeted inhibitor therapies.
Back to 2015 Annual Meeting Program
|