|
Back to 2014 Annual Meeting Posters
Prognostic Value of Additional Pancreatic Resection for Cancer Positive Cut Margins During Pancreaticoduodenectomy for Pancreatic Head Cancer
Satoshi Nara*, Kazuaki Shimada, Minoru Esaki, Yoji Kishi, Tomoo Kosuge
Hepatobiliary and Pancreatic Surgery Division, National Cancer Center Hospital, Tokyo, Japan
Background: Invasive ductal carcinoma of the pancreas often shows microscopic infiltration in the peripheral pancreatic parenchyma. Because this infiltration is difficult to recognize on preoperative imaging, invasive cancer at the pancreatic cut margin may be observed during pancreatectomy. However, the prognostic significance of additional pancreatic resection to achieve a final negative margin has not been determined.
Patients and methods: We retrospectively reviewed the records of 308 consecutive patients who underwent pancreaticoduodenectomy (PD) for pancreatic cancer, excluding invasive intraductal papillary mucinous carcinoma, at our hospital from 2000 to 2012. All patients underwent intra-operative frozen section analysis (IOFSA) of the pancreatic stump, with the need for additional pancreatic resection determined by the operating surgeon. Patients who underwent R2 resection, were positive for lavage cytology or para-aortic lymph node metastasis, received preoperative chemotherapy, or died in-hospital were excluded. Based on the final pathologic diagnosis of pancreatic cut margins, patients were divided into three groups: initial margins negative for invasive cancer (Group A); initial margins positive for invasive cancer, but negative after additional pancreatic resection (Group B); and final margins positive for invasive cancer (Group C). Patients who required conversion to total pancreatectomy (TP) were included in Group B. The clinicopathological characteristics and prognoses of the three groups were compared.
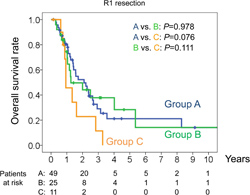
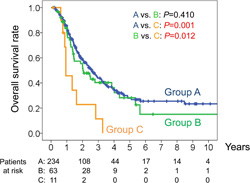
Results: IOFSA of the initial pancreatic stump showed that 71 patients harbored invasive cancer, 20 had PanIN3 and 25 had PanIN1 or 2. Additional pancreatic resection was performed in 99 patients, with 76 patients undergoing one, 14 undergoing two, four undergoing three, and five undergoing four or more resections. Eight patients required conversion to TP. IOFSA results were inconsistent with the final pathological diagnosis in 7 patients. Groups A, B and C consisted of 234, 63 and 11 patients, respectively, with median survival times of 31, 24, and 11 months, respectively, and 3-year survival rates of 44%, 40%, and 11%, respectively (A vs. B; P=0.410, A vs. C; P=0.001, B vs. C; P=0.012, Figure 1). Patients who underwent TP had a median survival time of 24 months and a 3-year survival rate of 43%. Rates of lymph node metastasis, R1 resection, portal vein resection and severe perineural invasion were significantly higher in Groups B and C than in group A. Survival was similar among the 85 patients in Groups A, B and C who underwent R1 resection (Figure 2).
Conclusion: Pancreatic margin status during PD should be confirmed, even if a curative resection is macroscopically expected. Additional pancreatic resection to achieve negative cut margins may improve postoperative survival.
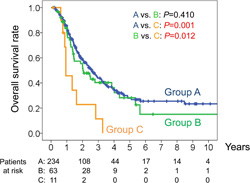 Figure 1 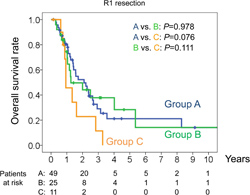 Figure 2
Back to 2014 Annual Meeting Posters
|