|
Back to 2014 Annual Meeting Posters
Esophageal Adenocarcinoma Identified in Consecutive Patients Undergoing Laparoscopic Roux-en-Y Gastric Bypass
Halle B. Ellison*1, Anna R. Ibele1, Anthony Petrick1, Michael Friscia2
1General Surgery, Geisinger Medical Center, Danville, PA; 2Thoracic Surgery, Geisinger Medical Center, Danville, PA
More than one third of Americans are obese. Obesity is a risk factor for gastroesophageal reflux disease (GERD) and esophageal adenocarcinoma (EA). Obesity is one of the fastest growing diseases and the incidence of EA is increasing faster than any other malignancy in the US. The only durable treatment for obesity and its comorbid conditions is bariatric surgery. There is no consensus among bariatric surgeons regarding the role of screening endoscopy (EGD) in patients with GERD prior to bariatric surgery.
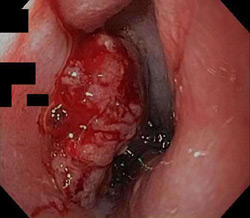
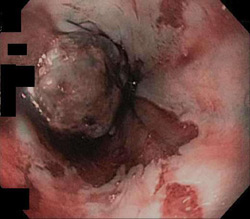
Two cases of incidental EA were identified by completion EGD following laparoscopic Roux-en-Y gastric bypass (LRYGB). EGD was done for anastomotic surveillance and provocative leak testing. Esophageal masses were identified and biopsies demonstrated adenocarcinoma.
The first patient is a 66 year old man with a body mass index (BMI) of 48 and no history of GERD. He quit smoking 13 years prior to evaluation. He was found to have T1bN0M0 EA. Laparoscopic transhiatal esophagectomy (LTHE) was completed three months after LRYGB during which he lost 46 pounds. Final pathology revealed high-grade dysplasia arising in Barrett's esophagus. Length of stay was six days. His postoperative course was complicated by transient recurrent laryngeal nerve palsy and anastomotic stricture. Six months post resection his hoarseness and dysphagia had resolved and his BMI was 31.
The second patient is a 49 year old man with a BMI of 45 and GERD. He used tobacco but quit two years prior to evaluation. He had T1bN1M0 EA and was treated with neoadjuvant carboplatin, paclitaxel and radiation. He lost 76 pounds in five months prior to LTHE. He had a complete pathologic response to neoadjuvant therapy. Length of stay was six days. He had an anastomotic leak which healed with stent placement. At follow up two months post resection his BMI was 30.
In both cases, LTHE was completed using the gastric remnant as conduit; the biliopancreatic limb was divided proximal to the jejunojejunostomy and anastomosed to the proximal roux limb to complete the reconstruction.
Obesity is a risk factor for GERD and EA. The role of EGD prior to bariatric surgery is unclear. Our group has performed over 4000 LRYGB with completion EGD prior to these two cases. Studies have demonstrated routine EGD prior to bariatric surgery may diagnose foregut pathology; however, few of the findings alter the planned treatment. The cost effectiveness of this strategy is questionable. There are reports of EA developing after bariatric surgery; however, we found no previous case reports of EA identified at LRYGB. LTHE is feasible after LRYGB. The conditioning of the gastric conduit and preoperative weight loss may be technically beneficial.
Esophageal cancer in patients undergoing bariatric surgery is rare. It may be beneficial to define selection criteria for patients who may benefit from routine preoperative EGD.
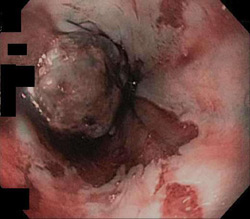 Patient One 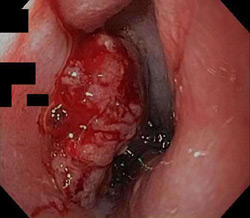 Patient Two
Back to 2014 Annual Meeting Posters
|