|
Back to 2014 Annual Meeting Posters
Learning Curve for Combined Thoracoscopic and Laparoscopic Robotic-Assisted Minimally Invasive Esophagectomy Using a Four-ARM Platform
Inderpal S. Sarkaria*, Nabil P. Rizk, Arjun Chandrasekaran, Manjit Bains, David J. Finley, Prasad S. Adusumilli, David R. Jones, James Huang, Valerie W. Rusch
Thoracic Service, Department of Surgery, Memorial Sloan-Kettering Cancer Center, New York, NY
Purpose: Robotic-assisted minimally invasive esophagectomy (RAMIE) using a 4-arm platform is a complex operation requiring a combined laparoscopic and thoracoscopic approach. Our objective was to evaluate the learning curve for this procedure using a dedicated operative team and a two-surgeon approach.
Methods: We conducted a prospective observational study of sequential patients undergoing RAMIE from 1/25/2011 to 10/22/2012. Demographics, operative times and peri-operative outcomes were recorded.
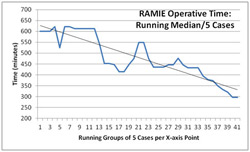
Results: 45 patients underwent RAMIE during the study period. Overall and inter-tertile patient demographics and outcomes are summarized in Table 1. Median estimated blood loss, median hospital length of stay (LOS), conversions rates, median operative times, and major complications (≥ grade 2 as defined by the Common Terminology Criteria for Adverse Events v. 3.0) decreased during the study period. Running median operative time per five cases is shown in Figure 1. There was one death (2.2%) within 90 days of surgery.
Conclusions: RAMIE is a complex procedure with short-term outcomes comparable to open and standard minimally invasive procedures. Using a dedicated operative team and a two surgeon approach, we estimate that a learning curve of 30-35 cases is required to achieve acceptable outcomes. Table 1. Patient overall and inter-tertile demographics and short-term outcomes. | Demographic/data point | Overall | First one-third | Second one-third | Third one-third | | Patients, no. | 45 | 15 | 15 | 15 | | Mean age, years | 62 (37-83) | 62 | 60 | 62 | | Male, % | 75 | | | | | Adenocarcinoma, % | 84 | | | | | Induction chemoradiation, % | 73 | | | | | Ivor-Lewis, % | 75 | | | | | Complete resection (R0), % | 81 | | | | | Median estimated blood loss, cc | 250 (50-700) | 350 | 300 | 200 | | Median lymph nodes, no. | 21 (10-56) | 21 | 19 | 24 | | Conversion to open surgery, % | 24 | 33 | 13 | 7 | | Last 5 cases | 0 | | | | | Median operative time, min | 468 (283-807) | 603 | 452 | 373 | | Last 5 cases | 297 (283-374) | | | | | Median length of stay, days | 10 (7-70) | 10 | 10 | 9 | | Last 5 cases | 9 (7-9) | | | | | Complications (CTCAE v3.0) | | | | | | Grade II | 12/45 (27%) | 40% | 20% | 20% | | Grade III-IV | 8/45 (17%) | 33% | 27% | 0% | | Grade V (death) | 1/45 (2.2%) | 7% | 0% | 0% | | Anastomotic leak ≥ grade II | 4/45 (9%) | 13% | 0% | 7% |
 Figure 1. Running median operative time per five cases.
Back to 2014 Annual Meeting Posters
|