|
 |
Back to 2014 Annual Meeting Posters
The Effect of Surgical Approach on the Use of Adjuvant Chemotherapy Following Low Anterior Resection for Rectal Cancer
Asvin M. Ganapathi*, Brian R. Englum, Paul J. Speicher, Anthony Castleberry, Julie K. Thacker, Christopher R. Mantyh, John Migaly
Division of Surgical Oncology, Department of Surgery, Duke University Medical Center, Durham, NC
Background:
Adjuvant chemotherapy (AC) following proctectomy for locally advanced rectal cancer is recommended by current treatment guidelines. While laparoscopic low anterior resection (LAR) reduces peri-operative complications, no study has examined the effect of surgical approach on the potential to receive AC. This study aims to determine if a laparoscopic, compared to open, approach for LAR leads to increased use of AC.
Methods:
Using the National Cancer Data Base, which documents patient demographics, tumor characteristics and survival outcomes for >70% of United States cancer cases, all patients with locally advanced rectal cancer (node positive or T3) from 2010-2011 were identified. Patients were stratified based on surgical approach, laparoscopic or open, and the primary outcomes of interest were receiving AC at anytime and within 90 days. The Chi-square test or Student's t-test were used for comparisons between the groups for categorical and continuous variables respectively. To adjust for non-random treatment choices a propensity analysis with inverse probability weighting (IPW) was conducted. Following adjustment, a weighted logistic regression analysis was done to examine the independent effect of surgical approach on likelihood to receive AC.
Results:
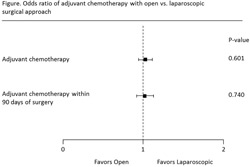
N=10,572 patients with locally advanced rectal cancer were identified with 66.3% receiving an open LAR (n=7,011) and 33.7% (n=3,561) having a laparoscopic LAR. Unadjusted analysis revealed that a laparoscopic approach was more common in patients who were younger, of white race, who had private insurance, who had smaller tumors, clinical stage T1, T2, or N0, or who had not received neoadjuvant chemo or radiation therapy, however IPW adjustment eliminated these differences (Table). Prior to adjustment, patients with a laparoscopic LAR were more likely to receive AC (45.3% vs. 41.5% in open patients; p<0.01) and to have AC earlier following surgery (52.7 days v. 56.2 days for open patients; p<0.01). While no significant difference was observed in rates of AC following IPW adjustment (43.1% v. 42.6% for laparoscopic compared to open; p=0.60), the time to AC remained shorter for laparoscopic LAR patients (52.6 days vs. 55.8 days for open approach; p=0.01) (Table). Weighted logistic regression analysis confirmed that surgical approach was not independently associated with receiving AC at anytime (Odds ratio [OR] = 1.02; p=0.60) or within 90 days (OR=1.02; p=0.74) (Figure).
Conclusions:
Use of AC following LAR for locally advanced rectal cancer confers a survival advantage and is recommended by current guidelines. While surgical approach was not associated with receiving AC, patients who had a laparoscopic LAR received AC earlier than those undergoing open LAR. Additional analysis of the effect of surgical approach for LAR on long-term survival and disease free interval is necessary. Table: Unadjusted and IPW Adjusted Patient and Operative Characteristics and Short-Term Outcomes | Unadjusted | After IPW Adjustment | | Variable | Open (n=7,011) | Laparoscopic (n=3,561) | P-Value | Open (n=7,011) | Laparoscopic (n=3,561) | P-Value | | Age, years +/- SD | 62.2+/-13.3 | 61.3+/-13.2 | 0.002 | 61.9+/-13.3 | 61.9+/-13.2 | 0.909 | | Female Sex | 41.9% | 40.6% | 0.195 | 41.4% | 41.4% | 0.945 | | White Race | 85.6% | 87.2% | 0.008 | 86.1% | 86.2% | 0.994 | | Charlson Comorbidity Score | | | 0.226 | | | 0.976 | | 0-1 | 94.3% | 95.1% | | 94.5% | 94.5% | | | 2+ | 5.7% | 4.9% | | 5.5% | 5.5% | | | Treatment facility | | | <0.001 | | | 0.948 | | Comprehensive Community Cancer Program | 56.4% | 60.5% | | 57.9% | 58.2% | | | Academic/Research Program | 31.8% | 32.5% | | 32.0% | 31.8% | | | Insurance | | | <0.001 | | | 1 | | Private | 46.3% | 53.7% | | 48.8% | 48.7% | | | Medicare | 40.7% | 36.9% | | 39.4% | 39.4% | | | Other | 13.0% | 9.4% | | 11.8% | 11.9% | | | Tumor Size ≥ 5.0 cm | 39.2% | 34.6% | <0.001 | 37.7% | 37.9% | 0.997 | | Clinical T Stage | | | <0.001 | | | 0.996 | | 1-2 | 17.6% | 23.4% | | 19.4% | 19.2% | | | 3-4 | 82.4% | 76.6% | | 80.6% | 80.8% | | | Clinical N Stage | | | 0.028 | | | 0.953 | | 0 | 62.1% | 64.3% | | 62.8% | 62.5% | | | 1 | 31.4% | 30.3% | | 31.1% | 31.2% | | | 2 | 6.5% | 5.4% | | 6.1% | 6.3% | | | Neoadjuvant Radiation Therapy | 49.7% | 43.1% | <0.001 | 47.6% | 47.9% | 0.789 | | Neoadjuvant Chemotherapy | 49.9% | 42.5% | <0.001 | 47.5% | 47.7% | 0.845 | | OUTCOMES | | | | | | | | Adjuvant Chemotherapy | 41.5% | 45.3% | <0.001 | 42.6% | 43.1% | 0.601 | | Days From Surgery to Adjuvant Chemotherapy (+/- SD) | 56.2+/-36.4 | 52.7+/-30.7 | 0.008 | 55.8+/-35.7 | 52.6+/-30.9 | 0.014 |
Back to 2014 Annual Meeting Posters
|