|
 |
Back to 2014 Annual Meeting Posters
Laparoscopic Versus Open Appendectomy: a Tri-State, 6-Year Analysis of Trends & Outcomes
Cheguevara Afaneh*1, Jonathan Abelson1, Gregory Giambrone2, Kseniya Slobodyanyuk2, Jonathan Eskreis-Winkler2, Akshay U. Bhat3, Ramin Zabih3, Alfons Pomp1, Peter Fleischut2
1Surgery, NY Presbyterian Hospital, New York, NY; 2Anesthesiology, NY Presbyterian Hospital, New York, NY; 3Cornell University, Ithaca, NY
Introduction: Multiple single-institutional trials comparing laparoscopic appendectomy (LA) to open appendectomy (OA) have been reported over a single year, including several national reports; however, the results have been conflicting. We report outcomes comparing LA to OA from a state-wide level over a 6 year period.
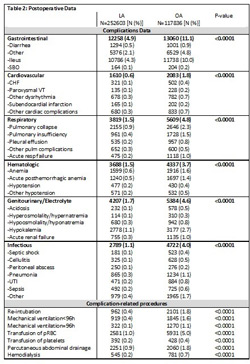
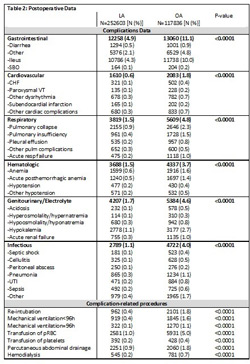
Methods: Using the State Inpatient Databases (SID), Healthcare Cost and Utilization Project, Agency for Healthcare Research and Quality, we retrospectively reviewed outcomes of all LA and OA performed from 2006 to 2011 in California, Florida, and New York. Preoperative variables, including gender, age distribution, insurance data, and diagnoses were compared. Outcomes specifically focused on length of stay (LOS), complications as graded by the Clavien-Dindo classification system, complication-related procedures, and mortality (stratified by year).
Results: A total of 363,737 appendectomies were performed with a total of 252,603 LAs and 117,836 OAs performed over the study period. Comparing OA to LA, a higher proportion of OA patients were male (P<0.0001), older (P<0.0001), and insured by Medicare or Medicaid (P<0.0001, Table 1). Moreover, a higher proportion of the OA group had co-morbidities, including diabetes mellitus type II, hypertension, and atrial fibrillation (P<0.0001). Patients with peritonitis or peritoneal abscesses were more likely to undergo OA (P<0.0001). The LOS was significantly longer in the OA over every time period measured (P<0.0001). The conversion rate from LA to OA was 12.84%. Discharges in the OA group had a higher proportion of the complications in each of the categories listed in Table 2. Furthermore, when patients in the OA developed a complication, they were more likely to need an additional intervention or procedure (Clavien-Dindo Grade >II). Overall in-hospital mortality was significantly higher in the OA compared to LA (0.48% vs. 0.06%, respectively; P<0.0001).
Conclusion: LA had significantly less morbidity, mortality, and shorter hospitalizations compared to OA. However, patients may be preselected to undergo OA given age, co-morbidities and preoperative diagnosis, which may also predispose towards more morbidity and mortality. The SID has important limitations; therefore, further analyses are necessary to identify the full impact of these findings.

Back to 2014 Annual Meeting Posters
|