|
 |
Back to 2014 Annual Meeting Posters
The Impact of Pancreatic Fistula Grade C on Survival After Pancreatic Resection; Analysis of 1,015 Patients With Pancreatic Cancer in Multicenter Study
Manabu Kawai*1,8, Yoshiaki Murakami2,8, Masaji Tani1,8, Seiko Hirono1,8, Ken-Ichi Okada1,8, Fuyuhiko Motoi3,8, Michiaki Unno3,8, Masayuki Sho4,8, Yoshiyuki Nakajima4,8, Kenichiro Uemura2,8, Sohei Satoi5,8, a-Hon Kwon5,8, Ippei Matsumoto6,8, Tadahiro Goto6,8, Goro Honda7,8, Masanao Kurata7,8, Hiroki Yamaue1,8
1Second Department of Surgery, Wakayama Medical University, Wakayama, Japan; 2Department of Surgery, Institute of Biomedical and Health Sciences, Hiroshima University, Hiroshima, Japan; 3Division of Gastroenterological Surgery, Department of Surgery, Tohoku University, Sendai, Japan; 4Department of Surgery, Nara Medical University, Nara, Japan; 5Department of Surgery, Kansai Medical University, Osaka, Japan; 6Division of Hepato-Biliary-Pancreatic Surgery, Department of Surgery, Kobe University Graduate School of Medicine, Kobe, Japan; 7Department of Surgery, Tokyo Metropolitan Cancer and Infectious diseases Center Komagome Hospital, Tokyo, Japan; 8Multicenter Study Group of Pancreatobiliary Surgery (MSG-PBS), Japan, Japan
Background: Several studies demonstrated that postoperative complications after pancreatic resection for pancreatic cancer adversely affect survival outcome. Pancreatic fistula grade C is one of the most serious complications after pancreatic resection. However, it remains unclear whether pancreatic fistula grade C affects long-term outcome after resection for pancreatic cancer.
Aims: The aim of this study is to elucidate the adverse effect of pancreatic fistula grade C on recurrence and survival after resection for pancreatic cancer by a survey of high volume center of pancreatic resection in Japan.
Methods: Medical records were reviewed in 1,015 patients with pancreatic cancer who underwent pancreatic resection between 2001 and 2010 at 7 high-volume surgical institutions in Japan. Pancreatic fistula was defined based on the International Study Group on Pancreatic Fistula (ISGPF) guideline.
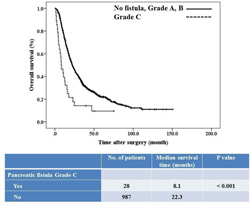
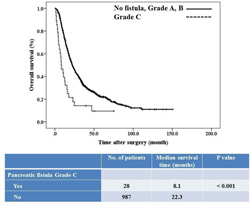
Results: Overall morbidity following pancreatic resection was 42.6%, and 30-day mortality was 0.3%. Pancreatic fistula occurred in 22.9% (232 of enrolled 1,015 patients) ; grade A 9.4%, grade B 10.7%, grade C 2.8%. Concerning with disease-free survival, patients with pancreatic fistula grade C had a significantly shorter time to recurrence than those without it (5.8 vs. 12.6 months, p=0.019). Concerning with overall survival, patients with pancreatic fistula grade C had a significantly poorer survival than those without it (8.1 vs. 22.3 months; median survival, 14.3 vs. 32.6% months; 3-year survival, p<0.0001). Pancreatic fistula grade C was an independent prognostic factor after multivariate analysis (hazard ratio 2.49; 95% confidence interval 1.56-3.96; P< 0.001). Moreover, independent prognostic significance was also detected for glasgow prognostic score (GPS) 2 (P=0.021), blood transfusion (P< 0.001), International Union Against Cancer (UICC) pT3 or T4(P= 0.003), pathological plexus invasion (P= 0.001), lymph node status (N1) (P= 0.024), no adjuvant therapy (P< 0.001). Furthermore, multivariate analysis demonstrated that independent risk factors for pancreatic fistula grade C was glasgow prognostic score (GPS) 2 (hazard ratio 5.37; 95% confidence interval 1.31-22.0; P=0.019) and male (hazard ratio 6.02; 95% confidence interval 1.77-20.5; P=0.004)
Conclusions: pancreatic fistula grade C had a significant impact on the long-term survival of patients with pancreatic cancer. The improvement of operative procedure or perioperative management to reduce the incidence of pancreatic fistula grade C may lead to a favorable survival in these patients.
Back to 2014 Annual Meeting Posters
|