|
 |
Back to 2014 Annual Meeting Posters
Impact of Preoperative Biliary Drainage on Short- and Long-Term Outcome After Pancreaticoduodenectomy for Cancer of the Head of Pancreas
Kenichiro Uemura*1,2, Yoshiaki Murakami1,2, Manabu Kawai1,3, Ken-Ichi Okada1,3, Ippei Matsumoto1,4, Sadaki Asari1,4, Sohei Satoi1,5, Hiroaki Yanagimoto1,5, Masayuki Sho1,6, Takahiro Akahori1,6, Goro Honda1,7, Masanao Kurata1,7, Fuyuhiko Motoi1,8, Michiaki Unno1,8
1Multicenter Study Group of Pancreatobiliary Surgery (MSG-PBS), Japan, Japan; 2Surgery, Hiroshima University, Hiroshima, Japan; 3Second Department of Surgery, Wakayama Medical University, Wakayama, Japan; 4Surgery, Kobe University, Kobe, Japan; 5Surgery, Kansai Medical University, Osaka, Japan; 6Surgery, Nara Medical University, Nara, Japan; 7Surgery, Komagome Hospital, Tokyo, Japan; 8Surgery, Tohoku University, Sendai, Japan
Background: Recent reports have suggested that preoperative biliary drainage (PBD) increases the perioperative morbidity rate of pancreaticoduodenectomy (PD). However, the effect of PBD on long-term outcome after PD for pancreas head cancer (PHCA) still remains unclear.
Aims: To evaluate the impact of PBD on short- and long-term surgical outcome in patients with PHCA undergoing PD.
Methods: Retrospective analysis was performed in 932 patients with PHCA who underwent PD with R0 or R1 resection between 2001 and 2012 at 7 high-volume surgical institutions in Japan.
Results: 166 patients (18%) underwent preoperative percutaneous transhepatic biliary drainage (PTBD), 407 patients (44%) underwent preoperative endoscopic biliary drainage (EBD), and 359 patients (39%) had no-PBD. The incidence of infectious complications after PD in the patients who underwent preoperative PTBD was significantly higher than those in the patients who had EBD and no-PBD (30%, 20%, and 18%, p=0.010). There were no differences in the incidence of postoperative pancreatic fistula (12%, 9%, and 9%; P=0.498), severe complication (25%, 21%, and 17%; p=0.117), and 30-day mortality (0%, 0.9%, and 0.3%; P=0.169) among three groups.
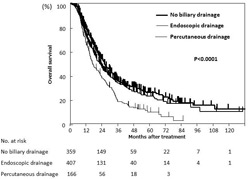
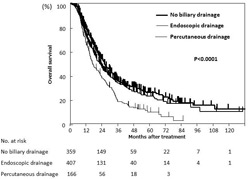
Patients who underwent preoperative PTBD had significantly poorer survival than those with EBD and no-PBD (16.7 months, 22.3 months, and 25.7 months; p<0.0001) (Fig). Multivariate analysis revealed that independent prognostic factors included age (P=0.003), blood loss (P<0.001), tumor size (p=0.016), tumor differentiation (p<0.001), lymph node metastasis (p<0.001), surgical margin status (p=0.004), adjuvant chemotherapy (p<0.001), and type of preoperative biliary drainage (p=0.015). Furthermore, preoperative PTBD group had significantly higher incidence of peritoneal metastasis as a primary site of recurrence compared with EBD and no-PBD group (26%, 14%, 16%; p=0.017). Multivariate analysis demonstrated that independent risk factors for peritoneal metastasis as a primary site of recurrence included surgical margin status (p<0.001), and preoperative PTBD (p=0.005).
Conclusions: Preoperative PTBD, but not EBD had negative impact on short- and long-term surgical outcome in the patients undergoing PD for PHCA. Poorer prognosis of the patient undergoing preoperative PTBD might be associated with peritoneal metastasis. These suggest that preoperative PTBD should be avoided whenever possible in patients with potentially resectable PHCA.
Back to 2014 Annual Meeting Posters
|