|
 |
Back to 2014 Annual Meeting Posters
Who Travels for Cancer Care? Regionalization of Pancreatectomy in Massachusetts
Lindsay a. Bliss*1, Theodore P. Mcdade3, Zeling Chau3, Jillian K. Smith3, Catherine J. Yang1, Sing Chau NG1, Bruce B. Cohen4, Giles F. Whalen3, Mark P. Callery2, Jennifer F. Tseng1
1Surgical Outcomes Analysis & Research, Beth Israel Deaconess Medical Center, Boston, MA; 2Surgery, Beth Israel Deaconess Medical Center, Boston, MA; 3Surgery, University of Massachusetts School of Medicine, Worcester, MA; 4Division of Research and Epidemiology, Massachusetts Department of Public Health, Boston, MA
Background: Improved outcomes for technically complex procedures have been reported for high-volume centers and surgeons. However, the magnitude and effect of regionalization of pancreatic cancer surgery has not been well characterized.
Methods: Retrospective observational cohort review of Massachusetts Department of Public health (MA-DPH) Inpatient Hospital Discharge Database (HDD). Admissions between 2005 and 2009 for pancreatic malignancy identified by ICD-9 were included. Patients without pancreatic resections or with missing or out-of-state ZIP codes were excluded. Hospitals were divided into high volume (≥11 cancer pancreatectomies annually) or low volume (<11 cancer pancreatectomies annually). Traveling distance was calculated as center-to-center geodetic distance between ZIP codes. Outcomes of interest included length of stay (LOS), perioperative mortality, hospital volume status, and distance traveled to treating hospital. Univariate analyses were performed for patient demographics. Multivariate logistic regression was used to identify independent predictors.
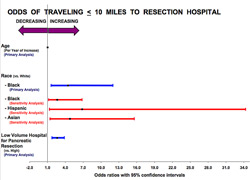
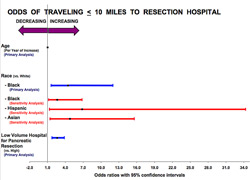
Results: 704 patients met inclusion criteria and were largely white (87.2%) with median age of 65 years. Median ZIP code income was $54,677. Distance traveled for resection varied from 0 to 112 miles (median 15.4). Median LOS was 8.0 days. Odds of traveling >10 miles for resection was higher among men (p=0.0319), patients less than 65 years of age (p=0.0392), and patients residing in ZIP codes with income >2x the poverty line (p=0.0130). Patients traveling more than 10 miles were more likely to receive care at high-volume hospitals. However, after adjustment, traveling for resection per se did not result in independently improved outcomes.
Conclusion: Most Massachusetts pancreatic cancer patients traveled more than 10 miles for resection. Patients who were younger, white, male, or residing in higher income areas were more likely to travel for care, suggesting demographic differences between travelers and nontravelers. Our data suggest some of the described volume effect on pancreatic cancer surgery may be due to patient selection rather than hospital or surgeon expertise.
Back to 2014 Annual Meeting Posters
|