|
Back to 2014 Annual Meeting Posters
Liver Transplantation for Unresectable Intrahepatic Cholangiocarcinoma: Improved Outcomes With Neoadjuvant Therapy
Alexandra Turner*, ADAM a. Golas, Matthew S. Johnson, Attila Nakeeb, Henry a. Pitt, Michael G. House
Surgery, Indiana University School of Medicine, Indianapolis, IN
Introduction: The incidence and mortality of intrahepatic cholangiocarcinoma (ICC) is increasing in the US and worldwide. Although complete surgical resection represents the only curative therapy for ICC, many patients present with advanced stage, unresectable disease. The use of neoadjuvant therapy prior to orthotopic liver transplantation (OLT) for ICC was recently demonstrated to improve disease-free survival compared to surgical resection in selected patients. The purpose of this study was to compare the long-term outcomes for patients with ICC treated with surgical resection, neoadjuvant therapy followed by OLT, or liver directed therapy in the form of hepatic artery embolization.
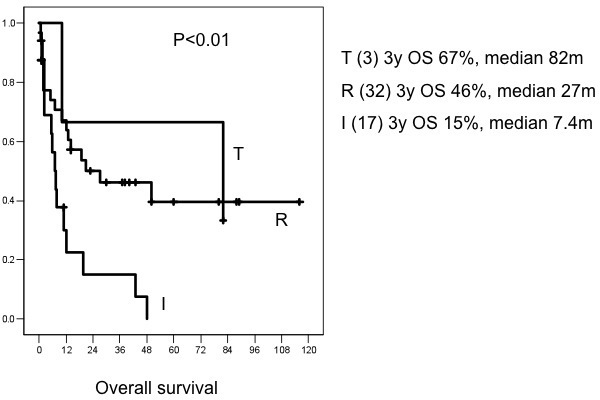
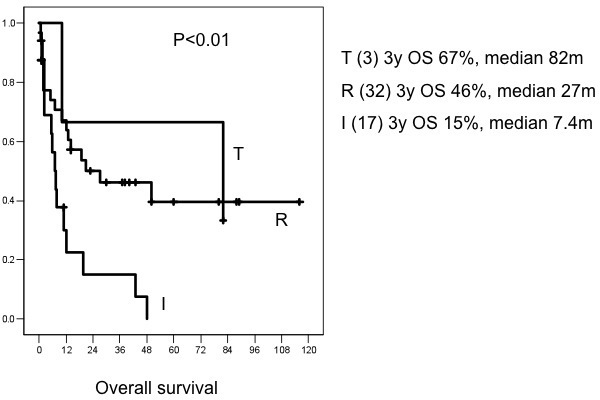
Methods: To ensure adequate follow-up, patients with ICC were reviewed at a single institution between January 2003 and December 2011. Clinical and pathologic data were collected retrospectively for patients who underwent either non-transplant resection (n=36), neoadjuvant therapy followed by OLT (n=3), or hepatic artery embolization (n=17). Overall survival was calculated from the date of operation or first treatment to the date of last follow-up or death. Actuarial survival was compared among the treatment groups with log-rank testing.
Results: Three year overall survival was 67% for patients after OLT, 46% after non-transplant resection, and 15% after hepatic artery embolization. Median survival was 82 months, 27 months and 7.4 months, respectively (p < 0.01, Figure). Median follow up was 47 months after OLT (1-79), 50 months after resection (1-116) and 5.9 months after embolization (0.6-48). Median tumor diameter was 6.5 cm (range, 1.8-18.2cm). A margin-negative (R0) resection was accomplished in only 11 pts (30%) within the non-transplant resection group; post-operative morbidity was observed in 23 patients (64%) after surgical resection.
Conclusions: OLT after neoadjuvant therapy for unresectable ICC is associated with significantly improved overall survival compared to other treatment modalities. OLT should be considered a treatment option for carefully selected patients with unresectable ICC.
Back to 2014 Annual Meeting Posters
|