|
Back to 2014 Annual Meeting Posters
Fibrosis, Cirrhosis and Mortality Following Hepatic Resection for Hepatocellular Carcinoma: Analysis of the National Cancer Data Base
Curtis J. Wray*, Tien C. Ko, Lillian Kao
Surgery, University of Texas Medical School at Houston, Houston, TX
Introduction: Underlying liver disease and portal hypertension limit surgical treatment options for hepatocellular carcinoma (HCC), as these patients are high-risk for complications. We hypothesize that hepatic fibrosis and cirrhosis increase the probability of post-resection 30-day mortality.
Methods: The National Cancer Data Base (NCDB) was queried for all cases of HCC from 1998-2011. Hepatic fibrosis was measured using the Ishak scale (0= no fibrosis and 1 = bridging fibrosis and cirrhosis). Comorbid conditions were classified using the Charlson/Deyo scores (0, 1, 2) and the model for end-stage liver disease (MELD) score was calculated as a measure of liver function. Hepatic resection was coded as segmentectomy, lobectomy or extended lobectomy. Patients undergoing liver transplantation and those without a fibrosis score were excluded. Outcomes of interest included 30-day readmission and 30-day mortality. Logistic regression was used to identify predictors of mortality. Receiver operating characteristic graphs and area under the curve (AUC) were used to validate the predictive accuracy of the models.
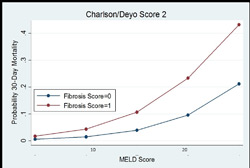
Results: Of 15901 HCC patients that underwent resection, 2304 had a fibrosis score; 103 patients (4.5%) died within 30 days following resection. The patients who died were older (66 vs. 62 years), had a Charlson/Deyo score >1 (64% vs. 50%), had hepatic fibrosis (51% to 37%), had a HCC stage>1 (66% vs. 56%) and underwent major anatomical resections (43% vs. 31%). On multiple regression analysis, predictors of mortality included Charlson/Deyo score 2 (OR 2.02, 95%CI: 1.19-3.43), fibrosis score 1 (OR 1.76, 95%CI: 1.12-2.80), MELD (2.68, 95%CI: 1.61-4.47) and anatomic lobectomy (OR 1.79, 95%CI: 1.13-2.83). Using this model, the probability of 30-day mortality (see figure) for a patient (Charlson/Deyo score 2) with a MELD score = 8 increases from 5.0% (95%CI: 0.4-9.6) to 11.4% (95%CI: 3.0-19.6) once fibrosis is detected. If MELD score is increased to 16, the probability rises from 8.5% without fibrosis to 19.8% with fibrosis (95%CI: 7.4-31.4). The AUCs for the models with and without fibrosis were 0.87 (95% CI: 0.82-0.93) and 0.84 (95% CI: 0.77-0.92) respectively.
Conclusion: The combination of underlying liver disease and comorbid conditions significantly increase the risk of 30-day mortality in hepatocellular carcinoma patients undergoing resection. The presence of bridging fibrosis and cirrhosis may not alter the surgical approach in lower risk (i.e. lower MELD score) patients. However, for patients considered borderline candidates for resection, a preoperative biopsy of the noncancerous hepatic parenchyma may provide additional prognostic information to both the surgeon and patient.
Back to 2014 Annual Meeting Posters
|