|
Back to 2014 Annual Meeting Posters
Colonic Lumen Obliteration Following Colonic Lavage Treatment for Infectious Colitis
Joy Hughes*, Stephanie Polites, Donald Jenkins, Mariela Rivera, Martin D. Zielinski
Mayo Clinic, Rochester, MN
Introduction: We present two cases of colonic lumen obliteration following colonic lavage treatment for infectious colitis. This complication of lavage therapy for Clostridium Difficile has not been previously described.
Cases: The first patient is a 52 year old woman who underwent diverting loop ileostomy and subsequent colonic lavage after failing medical treatment for fulminant C. difficile colitis. After two weeks of antegrade colonic lavage with Vancomycin, she was discharged. Prior to ileostomy takedown three months later, contrast enemas through rectum and distal limb of loop ileostomy revealed strictures at the descending and sigmoid colon and total lumen obstruction at the distal descending colon. She underwent resection of the descending and sigmoid colon and pathology revealed two strictures of the colonic lumen down to 0.3 cm.
The second patient is a 58 year old woman who underwent diverting loop ileostomy and colonic lavage for fulminant C. difficile colitis following an unrelated spine operation. She recovered and was discharged after two weeks of antegrade colonic lavage with Vancomycin and intravenous Metronidazole. Three months later colonoscopy revealed colitis with loss of vascularity, erythema, and friability of the mucosa, and endoscopy was aborted at the splenic flexure due to risks of perforation. Biopsies showed no evidence of infectious colitis, and diagnosis of diversion colitis was made. She underwent ileostomy takedown the following day. Postoperatively, she developed obstipation and abdominal pain with distension secondary to colonic obstruction. Operative exploration revealed ischemia secondary to transverse colon obstruction. An extended right hemicolectomy with ileostomy was performed. In preparation for reestablishment of intestinal continuity 3 months later, a contrast enema showed no evidence of obstruction with contrast terminating at the splenic flexure. At reoperation, however, when attempting to close the ileostomy, complete obliteration of the transverse colon lumen was found, necessitating completion transverse colectomy and ileo-left colonic anastomosis. Pathology revealed fibrous obliteration of the colonic lumen over a 7 cm segment.
Conclusion: Colonic lumen obliteration is a potential complication of antegrade colonic lavage with Vancomycin for C. difficile colitis. All patients who undergo this therapy for C. difficile colitis should have verification of pan- colonic luminal patency prior to consideration of reestablishment of intestinal continuity.
 First patient: Hypaque enema through distal limb of loop ileostomy revealed distal colonic obstruction. First patient: Hypaque enema through distal limb of loop ileostomy revealed distal colonic obstruction.
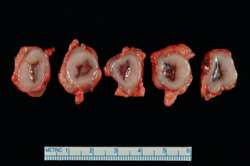
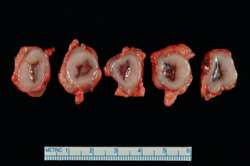
Second patient: Surgical specimens demonstrating colonic lumen obliteration.
Back to 2014 Annual Meeting Posters
|