|
 |
Back to 2014 Annual Meeting Abstracts
Clinical utility of using second-line Integrated Molecular Pathology testing in addition to First-line test algorithms to determine the malignant potential of pancreatic cysts (N=492)
Thomas E. Kowalski*1, David E. Loren1, Ali Siddiqui1, Howard Mertz3, Damien Mallat4, Nadim Haddad5, Nidhi Malhotra5, Brett Sadowski5, Mark J. Lybik6, Sandeep Patel7, Emuejevoke Okoh7, Laura Rosenkranz7, Michael Karasik8, Michael Golioto8, Jeffrey D. Linder9, Keith M. Callenberg11, Sara A. Jackson11, Marc F. Catalano10, Mohammad A. Al-Haddad2
1Thomas Jefferson University, Philadelphia, Pennsylvania, United States, 2Indiana University, Indianapolis, Indiana, United States, 3Nashville GI Specialists, Nashville, Tennessee, United States, 4Premier Gastroenterology of Texas, Dallas, Texas, United States, 5Georgetown University, Washington, District of Columbia, United States, 6Northside Gastroenterology, Indianapolis, Indiana, United States, 7University of Texas San Antonio, San Antonio, Texas, United States, 8Connecticut GI, PC, Hartford, Connecticut, United States, 9Digestive Health Associates of Texas, Dallas, Texas, United States, 10St. Luke's Medical Center, Milwaukee, Wisconsin, United States, 11RedPath Integrated Pathology, Pittsburgh, Pennsylvania, United States
Background & aims: Results of a multi-center pancreatic cyst study have shown that, when cytology results are non-malignant, integrated molecular pathology (IMP) can accurately differentiate cysts with low vs. high malignant potential by incorporating DNA molecular analyses with first-line tests (cytologic atypia, CEA, imaging).1 To assess the clinical utility of such testing in this study cohort, we compared the performance of IMP to that of algorithms integrating first-line test results.
Methods: 492 patients with non-malignant cytology at the time of IMP diagnosis (RedPath) were included. Patient outcomes were classified as benign or malignant based on subsequent surgical pathology (n=209) or clinical confirmation (n=283) including malignant cytology post-IMP testing, clinical cancer management, or 23+ months (23-92 months; median 35 months) imaging follow-up. Sendai 2012 radiographic and cytology criteria and CEA criteria (Sendai+CEA) were evaluated for their ability to discriminate high from low risk disease based on the presence of at least one concerning cyst feature: cyst size =3cm, solid component, main duct involvement, pancreatic duct dilation =1cm, severe cytologic atypia, or CEA =192. These criteria were also assessed using a support vector machine (SVM) learning algorithm trained with a radial basis function kernel using five-fold cross-validation.
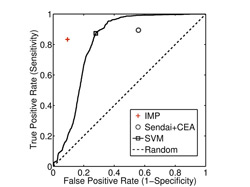
Results: Grouping patients as high risk (Sendai+CEA), based on the presence of at least one concerning first-line test, resulted in adequate sensitivity (59/66, 89%) for malignancy but at the expense of specificity (188/426, 44%) (Figure 1). Similar sensitivity (58/66, 88%) with improved specificity (311/426, 73%) was encountered when the SVM algorithm was used to determine the optimal combination of first-line test results that could best distinguish between patients with high and low risk of malignancy. By comparison, IMP was able to maintain statistically similar sensitivity (55/66, 83%)1 to both Sendai+CEA and SVM (both p>0.4) but with significantly improved specificity (386/426, 91%)1 compared to Sendai+CEA and SVM (both p<0.0001). Such differences were due to a 47% and 18% reduction in false positive diagnoses by IMP relative to Sendai+CEA and SVM, respectively.
Conclusions: While guideline recommended and, even, computer generated (SVM) algorithms of first-line tests often provide false evidence of high risk disease resulting in low specificity for malignancy, second-line IMP testing more accurately differentiates between patients at high and low risk of malignancy. As such, IMP testing can help to avoid unnecessary surgeries in patients destined for benign outcome, while providing reliable evidence for the need of surgery in patients who are at high risk of adenocarcinoma.
Reference: 1. Catalano, M, et al. Poster. ACG 2013; San Diego, CA.
Back to 2014 Annual Meeting Abstracts
|