|
Back to 2014 Annual Meeting Abstracts
Is Sacral Nerve Stimulation Here to Stay? Clinical Outcomes of a New Treatment for Fecal Incontinence
Ian M. Paquette*, Bobby L. Johnson, Martha Ferguson, Janice F. Rafferty
Colon and Rectal Surgery, University of Cincinnati College of Medicine, Cincinnati, OH
Purpose: Sacral nerve stimulation (SNS) was approved by the Food and Drug Administration for the treatment of fecal incontinence (FI) in 2011. Previous industry-sponsored trials have shown excellent clinical outcomes with this technique. The purpose of this study is to examine relevant clinical outcomes of patients treated during our initial experience with SNS.
Methods: A prospective database of all patients treated with SNS for FI by one of three Colorectal Surgeons was maintained starting in 2011. Patients with >2 episodes of FI per week with failure of conservative measures were eligible for SNS after a full discussion of options. Patients showing ≥50% improvement of symptoms during stage 1 test stimulation were offered chronic implantation of the InterStim system (Medtronic: Minneapolis, MN). Disease severity was tracked using the Wexner score, a validated FI scoring system with a score of 0 representing no symptoms, and 20 being the most severe disease.
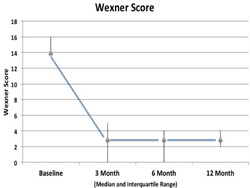
Results: One hundred and fifteen patients underwent stage 1 test stimulation with a 96.5% success rate. A total of 111 patients with a median age of 67 received a full system implantation. The median preoperative Wexner score was 14/20 (Interquartile range 14-16). The median Wexner score decreased to 3/20 at 3 months, and this result persisted at 12 months (Figure 1.) At 12 months, 93% of patients achieved at least a 50% improvement in Wexner Score (70% of patients achieved a 75-100% improvement). The most common adverse event was infection 4.4%. All but one patient with an infection required an explantation of the device. Two patients required revision of the electrode over time without the need to replace the entire system. A total of 54% of patients required programming changes in the office to obtain optimal results.
Conclusions: SNS is a safe and effective therapy for the treatment of FI. Postoperative patient surveillance is important, as many patients require programming changes, and some will require a lead revision over time.
 Figure 1: Change in Wexner Score over time (median and interquartile range)
Back to 2014 Annual Meeting Abstracts
|