|
Back to 2014 Annual Meeting Abstracts
Multivisceral Transplantation for Non-Resectable Abdominal Neuroendocrine Tumors
Richard S. Mangus*, Mary Maluccio, Chandrashekhar a. Kubal, Jonathan a. Fridell, a. Joseph Tector
Surgery, Transplantation Section, Indiana University, School of Medicine, Indianapolis, IN
Introduction
Neuroendocrine tumors (NETs) are slow growing tumors that are minimally responsive to chemotherapy and radiation therapy. These tumors may be cured with complete surgical resection. This paper presents a series of patients with metastatic or non-resectable NETs that were considered unresectable upon initial consideration, but subsequently underwent multivisceral transplant (MVT) with curative intent.
Methods
All patients at our center undergoing MVT for metastatic or non-resectable NET were included in this analysis. Diagnosis of NET required tissue confirmation. All patients underwent pre-transplant imaging including octreotide scan and PET CT. Patients with tumor outside of the intestine, pancreas, duodenum and liver were excluded for MVT. Immunosuppression included antibody-based induction and maintenance tacrolimus with low dose steroids.
Results
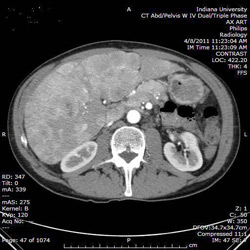
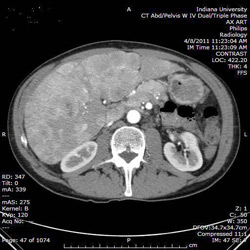
There were 120 full MVTs performed between 2004 and 2012, 13 of these were for NETs. All 13 NET patients had a primary abdominal tumor, with numerous metastatic liver lesions or a non-resectable primary encasing the root of the mesentery. A variety of pre-transplant therapies had been attempted on these patients including resection, chemotherapy and radiation therapy. There were 3 tumor types represented including carcinoid (4), islet cell (3), VIPoma (3). There were 3 with undetermined cell type. The MVT included resection of the native liver, stomach, duodenum, pancreas, spleen, intestine and right/transverse colon. The cluster graft included stomach, liver, duodenum, pancreas and intestine +/- colon. Lymph nodes in the retroperitoneum were resected during the operation in an attempt to remove all tumor. The image below demonstrates one of the transplanted patients with extensive liver involvement.
With a median follow up of 34 months (3-81), 8 of 13 patients are alive. There was 1 intraoperative death, and 5 of 12 surviving patients have recurrence (42%).
(a) 1 patient had recurrence in the transplant liver and died 10 months post-transplant of liver failure;
(b) 1 patient had asymptomatic recurrence in his mediastinal lymph nodes and died of neutropenic sepsis 17 months post-transplant;
(c) 3 patients have asymptomatic recurrence and are healthy and functional.
All eight living patients are healthy, enteral independent, at home with survival ranging from 3 to 81 months.
Conclusions
MVT for non-resectable abdominal NET may be a viable therapeutic option. We have several long-term, tumor free survivors who would otherwise have died from their terminal disease. Pre-transplant identification of occult or nodal disease using 68-Gallium based imaging is critical to assure complete tumor resection.
Back to 2014 Annual Meeting Abstracts
|