|
Back to 2014 Annual Meeting Abstracts
Importance of Lymph Node Involvement in Pancreatic Neuroendocrine Tumors: Impact on Survival and Implications for Surgical Resection
Thomas Curran*1, Barbara a. Pockaj2, Richard J. Gray2, Nabil Wasif2
1Surgery, Beth Israel Deaconess Medical Center, Boston, MA; 2Surgery, Mayo Clinic in Arizona, Scottsdale, AZ
BACKGROUND: Pancreatic neuroendocrine tumors (PNETs) are rare neoplasms with a variable clinical course. Data regarding predictors of lymph node involvement and the impact of nodal metastases on survival has been limited to single institution series. Similarly, the role of limited surgical resection, if any, in the management of PNETs is unknown. We aim to use a national cancer registry to: 1) identify factors associated with lymph node involvement 2) evaluate the effect of nodal metastases on survival and 3) identify a sub-set of patients suitable for limited resection.
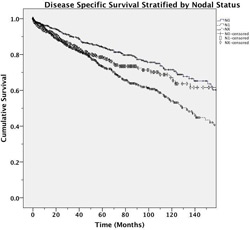
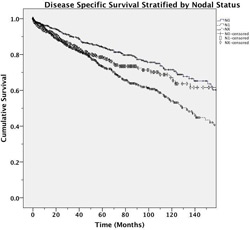
METHODS: All patients undergoing surgery for PNETs in the Surveillance, Epidemiology, and End Results (SEER) tumor registry from 1988 to 2010 were included. Pathologic lymph node status was classified as positive (N1), negative (N0) or unknown (Nx). Predictors of lymph node involvement were evaluated using multivariable logistic regression. Kaplan-Meier estimations were used to calculate unadjusted disease specific survival (DSS). Clinicopathologic predictors of DSS were determined via multivariable Cox regression analysis.
RESULTS: We identified 1,915 patients undergoing surgery for a PNET. Mean age was 55.9 (SD + 14.0) years and approximately half of the patients were female ( 48%). Most common tumor location was in the tail of the pancreas (34%) and the majority of the tumors were non-functional (62%). Breakdown by tumor grade was 49% grade I-II, 8% grade III-IV and 43% unknown. Tumor size was 0-2cm in 24%, 2-5cm in 42% and greater than 5cm in 34%. Lymph node status was N0 in 755 cases (39%), N1 in 735 cases (38%) and Nx in 425 cases (22%). Nodal positivity was associated with increasing tumor size (p<0.001) and grade (p <0.001). Median follow up was 40 months (IQR: 16-77 months) with 405 disease specific deaths. Unadjusted DSS at 5 years was 81% for N0, 74% for Nx and 69% for N1 respectively, (p <0.001). After adjustment for tumor size and grade, DSS was significantly decreased in N1 patients (HR: 1.57, 95%CI: 1.23-1.95). For patients who had at least one node examined and had low grade PNETs <1cm in size no nodal metastases were found.
CONCLUSIONS: High tumor grade and increasing size predicts nodal metastases in patients with PNETs. N1 status is independently associated with decreased DSS. Low-grade tumors less than 1cm are unlikely to have lymph node metastases, suggesting that enucleation or local resection may be oncologically safe in this patient subset.
Back to 2014 Annual Meeting Abstracts
|