|
 |
Back to 2014 Annual Meeting Abstracts
When Tissue Is the Issue: a New Device for Extracorporeal Hypothermic Perfusion of Intestinal Lumen and Vasculature Decreases the Rate of Necrosis During Graft Transportation
Raja R. Narayan*1,2, Roger Patron-Lozano1, Brian Loeb3, Kristi E. Oki3, Natalie Pancer4, Andrew Crouch4, Yusuf Chauhan4, Spencer Backus3, Richard E. Fan3, Joseph P. Zinter3, David C. Mulligan1, Sukru H. Emre1, John P. Geibel1, Manuel I. Rodriguez-Davalos1
1Department of Surgery, Yale University, New Haven, CT; 2Division of Applied Biostatistics and Epidemiology, Yale School of Public Health, New Haven, CT; 3Department of Mechanical Engineering, Yale University, New Haven, CT; 4Department of Biomedical Engineering, Yale University, New Haven, CT
Introduction:
Intestine remains the least commonly transplanted organ despite continuing need. With the advancement in immunosuppression and surgical techniques, the rate of successful small bowel transplants has increased however little has changed in the crucial intermediary step of keeping intestinal tissue viable. We sought to develop a device that could improve the preservation of the graft during this period by perfusing both the intestinal lumen and vasculature. We hypothesized that such treatment would lead to a lesser degree of necrosis than under the conditions of the current standard of care.
Methods:
Porcine small bowel was obtained using standard procurement techniques within 30 mins of circulatory arrest. Following dissection of the superior mesenteric artery and vein, each vessel was cannulated and attached to polyvinyl chloride (PVC) tubing. 2 meters of bowel from both the proximal and distal ends respectively were resected and stored in standard fashion as control. The remaining length of bowel was flushed with normal saline. Similar cannulation was performed as tubing was installed into the proximal and distal ends of the bowel. The graft, including the attached mesentery, was placed in a sterile bowel bag that was immersed in an ice bath within an insulated perfusion device. The two PVC tubes from the superior mesenteric vessels were attached to a self-priming, peristaltic pump to conduct cold normal saline in the anterograde direction. A separate identical pump was attached to the two PVC tubes in the intestinal lumen. Both legs of the experiment were allowed to run for 4 hours followed by formalin fixation.
Results:
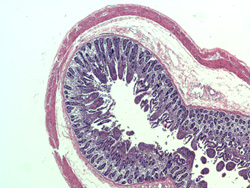
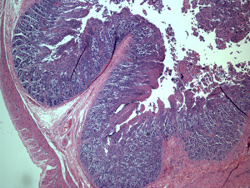
Samples from both the control and experimental specimens (Figures 1 and 2 respectively) were analyzed using Hematoxylin-Eosin staining. The control samples of the proximal and distal portions both showed increased epithelial inflammation with increased lymphocytes and eosinophils. There was focal early ulceration in the proximal portion. In contrast, the tissue samples that were continuously perfused with cold saline showed comparatively less inflammation and no detectable ulceration with overall reduced epithelial damage.
Conclusion:
The standard of care in preservation methods for intestinal grafts has not changed in the last two decades. Our results demonstrate that by using a perfusion system with a simple preservation solution, better histological results can be generated than by cold storage alone. These findings confirm that the continuous perfusion of small bowel with cold fluid aids in organ preservation by decreasing the rate of necrosis in intestinal tissue for transplantation. This presents opportunity for increasing the availability and quality of donor organs for transplantation by continuous perfusion of the mesentery and lumen of the intestine to allow for increased viability of the organ.
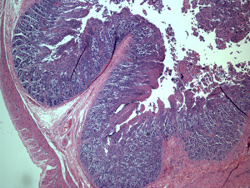 Figure 1. Control Intestinal Wall, Proximal Portion. 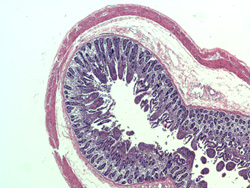 Figure 2. Experimental Intestinal Wall.
Back to 2014 Annual Meeting Abstracts
|