|
Back to 2014 Annual Meeting Abstracts
Development of a Prognostic Nomogram for the Need for Surgery After Endoscopic Balloon Dilatation of Ileocolic Anastomotic Stricture for Crohn's Disease
Lei Lian*, Luca Stocchi, Bo Shen, Xiaobo Liu, Feza H. Remzi
Cleveland Clinic, Cleveland, OH
Background
Endoscopic balloon dilatation has been increasingly used for the non-operative management of anastomotic strictures in patients with previous ileocolic resection for Crohn's disease. The aim of this study was to develop a nomogram to predict the need for surgery after initial endoscopic dilatation.
Patients and methods
Patients undergoing endoscopic dilatation of ileocolic anastomotic stricture between December 1998 and May 2013 were identified. Primary endpoint was need for bowel resection due to stricture, development of fistulizing disease, or perforation from endoscopic dilation. Cox proportional hazard regression model was used to assess factors significantly associated with the need for surgery within 5 years after initial dilation.
Results
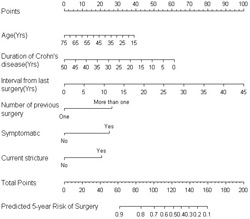
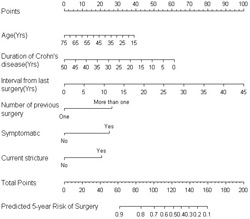
One hundred and eighty-four patients underwent a total of 454 endoscopic dilatations of ileocolic anastomosis (46.2% females, mean age 43, symptomatic stricture in 80%). Sixty-one patients (31.9%) eventually required surgery after a median follow up of 1.6 (0 - 13.3) years. Surgery was indicated for endoscopic perforation (n=5), technical failure (n=2), intractable stricture (n=42), development of intestinal fistula or abscess (n=8), and miscellaneous (n=4). The 5-year risk of surgery was 53.3% (95% confidence interval, 0.4- 0.6). A nomogram was developed using age, duration of Crohn's disease, interval from last surgery, multiple previous resections, symptomatic stricture, and the presence of concurrent stricture. The predictions from the nomogram appeared to be accurate and discriminating with a concordance index of 0.65.
Conclusion
The proposed nomogram is effective in predicting the 5-year probability of need for surgery to treat ileocolic strictures. It can be used to select patients for continued endoscopic dilatations vs. patients who should have surgery. Cox regression model of need for surgery | Variable | Hazard Ratio (95% confidence interval) | P value | | Age | 0.97(0.8-1.02) | 0.07 | | Duration of Crohn's disease | 0.96(0.93-1.03) | 0.07 | | Interval from last surgery | 1.07(1.03-1.12) | 0.001 | | Multiple previous surgery | 2.23(1.27-3.94) | 0.005 | | Symptomatic stricture | 2.20(0.97-4.97) | 0.06 | | Concurrent stricture | 2.0(1.04-3.88) | 0.04 |
Back to 2014 Annual Meeting Abstracts
|