|
Back to 2014 Annual Meeting Abstracts
Robotic Low Anterior Resection for Rectal Cancer and Short-Term Oncologic Outcomes
Paul J. Speicher*, Brian R. Englum, Asvin M. Ganapathi, Christopher R. Mantyh, John Migaly
Surgery, Duke University Medical Center, Durham, NC
Background:
Laparoscopic low anterior resection (LLAR) is considered an acceptable approach to rectal cancer. Due to limited oncologic and patient outcomes data, however, robotic low anterior resection (RLAR) remains more experimental. This study compared 30-day outcomes and pathologic surrogates of oncologic results between rectal cancer patients undergoing either RLAR or LLAR.
Methods:
All rectal cancer patients in the National Cancer Database (NCDB) undergoing RLAR or LLAR from 2010-2011 were stratified by operative approach. The NCDB collects data from more than 1,500 cancer centers across the United States and Puerto Rico, and is estimated to capture approximately 70 percent of all newly diagnosed cases of colorectal cancer. Predictors of RLAR were modeled with multivariable logistic regression. Groups were matched on propensity to undergo RLAR using a 2:1 nearest-neighbor matching algorithm. Primary oncologic endpoints included lymph node (LN) retrieval and margin status, while secondary 30-day outcomes were mortality, hospital length of stay, and unplanned readmission rates. Group characteristics were compared pre- and post-matching using Pearson's chi-square and one-way ANOVA.
Results:
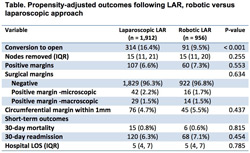
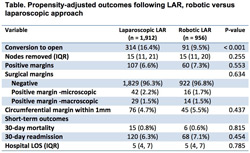
6,403 patients met inclusion criteria, of which 956 (14.9%) underwent RLAR. Baseline characteristics between groups were highly similar, except that RLAR patients were more likely to be treated at academic centers, to receive neoadjuvant therapy, had higher T-stage, and longer time from diagnosis to surgery (all p values <.001). Neoadjuvant therapy and treatment at an academic/research center remained the only significant predictor of robotic use following multivariable adjustment. Following propensity adjustment, RLAR was associated with reduced risk of conversion to open (9.5 vs. 16.4%, p<.001). There were no significant differences in LN retrieval, margin status, 30-day mortality, unplanned readmission, or hospital length of stay (Table).
Conclusions:
In the largest series to date using a nationwide clinical database, we demonstrated equivalent perioperative safety and patient outcomes for robotic compared to laparoscopic LAR in the setting of rectal cancer. While the robotic approach required significantly fewer conversions to open, surrogates for proper oncologic surgery were nearly identical between the two approaches, suggesting that a robotic approach to colorectal cancer may be a suitable alternative. Further studies comparing long-term cancer recurrence and survival should be performed.
Back to 2014 Annual Meeting Abstracts
|