|
 |
Back to 2014 Annual Meeting Abstracts
Timing of Discharge: a Key to Understanding the Reason for Readmission After Colorectal Surgery
Kristin N. Kelly*, James C. Iannuzzi, Christopher T. Aquina, Christian P. Probst, Katia Noyes, John R. Monson, Fergal Fleming
Surgical Health Outcomes and Research Enterprise, Department of Surgery, University of Rochester, Rochester, NY
PURPOSE:
In the current healthcare environment there is an ever-present pressure to improve the value of care delivery. As a result, many question if patients are being discharged too soon as a means of reducing cost. There is a growing interest in understanding the delicate balance between appropriate hospital length of stay (LOS) and prevention of unnecessary readmissions. This study examines the relationship between postoperative LOS and unplanned readmission after colorectal resection and explores whether patients discharged earlier are at risk for different complications necessitating readmission.
METHODS:
Patients undergoing colorectal resection were selected by CPT code from the 2012 ACS NSQIP database. Only patients surviving to discharge with a postoperative LOS 1-14 days in duration were included allowing for at least 2 weeks of follow up. Patients were stratified by LOS quartile: 1-3 days, 4-5 days, 6-7 days, and ≥8 days. Kaplan Meier analysis was used to examine the relationship of patient and perioperative characteristics with 30-day unplanned readmission. Factors with a p<0.1 were included in the Cox proportional hazards model. Subsequently, ICD-9 codes were used to group reasons for unplanned readmission. Chi-square analysis compared LOS and patient and perioperative factors with the primary reason for readmission. Factors with a p<0.1 were included in a multivariable logistic regression for each readmission reason.
RESULTS:
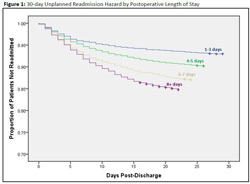
For 33,033 patients undergoing colorectal resection, the overall 30-day unplanned readmission rate was 11% ranging from 7% in patients with a 1-3 day LOS to 15% in patients with a ≥8 day LOS. Mean postoperative LOS was 5.9 days. After adjusting for patient and perioperative factors, greater postoperative LOS was associated with higher relative hazard of readmission (Figure 1). The most common reported reasons for readmission were intra-abdominal infection, wound complications, and ileus/obstruction (Table 1). Patients with a 1-3 day LOS were more likely than patients with longer LOS to be readmitted with ileus/obstruction (OR:1.7 CI:1.2,2.4 p=0.01) and pain (OR:1.8 CI:1.0,3.4 p=0.05). LOS was not significantly associated with readmission for intraabdominal infection or medical complications.
CONCLUSIONS:
After adjusting for patient and perioperative characteristics this study found longer LOS was independently associated with increased unplanned 30-day readmissions following colorectal resection. Patients with a complicated hospital course continue to be high risk post-discharge, while straightforward early discharges have a different readmission risk profile. More targeted readmission prevention strategies, like ensuring appropriate bowel function and pain regimens for patients discharged earlier, are critical to focusing resource utilization for patients following colorectal surgery. Table 1: Multivariable analysis of Association between Length of Stay Quartile and Readmission Reason | | 1-3 days LOS | 4-5 days LOS | 6-7 days LOS | | Readmission Reason | N (% of all readmissions) | Adjusted OR (CI) | p-value | Adjusted OR (CI) | p-value | Adjusted OR (CI) | p-value | | Intra-abdominal infection | 505 (13.5) | 0.85 (0.60, 1.21) | 0.38 | 0.95 (0.73, 1.23) | 0.71 | 0.92 (0.70, 1.20) | 0.85 | | Wound complication | 500 (13.4) | 0.98 (0.66, 1.45) | 0.91 | 1.23 (0.94, 1.62) | 0.13 | 1.35 (1.05, 1.75) | 0.02 | | Ileus or Obstruction | 401 (10.7) | 1.65 (1.15, 2.37) | 0.01 | 1.11 (0.82, 1.50) | 0.49 | 0.99 (0.73, 1.35) | 0.95 | | Medical complication | 255 (6.8) | 0.80 (0.47, 1.38) | 0.43 | 0.88 (0.61, 1.28) | 0.51 | 0.86 (0.61, 1.22) | 0.40 | | Pain | 141 (3.8) | 1.83 (0.99, 3.36) | 0.05 | 1.32 (0.80, 2.18) | 0.27 | 1.22 (0.73, 2.05) | 0.45 |
LOS: Postoperative Length of Stay; OR: Odds Ratio; CI: 95% Confidence Interval *LOS ≥8 days used at the reference category in all models. Other less frequent reasons for readmission included sepsis, dehydration, hemorrhage, PE/DVT, other GI complaints, and other/unknown Intra-abdominal infection model also adjusted for age, sex, diabetes, ASA class, functional status, cardiac comorbidity, bleeding disorder, preoperative sepsis/SIRS, anemia, wound class, emergency cases, discharge to non-home location, and minor pre-discharge complications. Wound complication model also adjusted for age, Hispanic ethnicity, race, obesity, smoking, pulmonary comorbidity, hepatic insufficiency, renal insufficiency, open surgery, and minor/major pre-discharge complications. Ileus/obstruction model also adjusted for obesity, diabetes, ASA class, cardiac comorbidity, renal insufficiency, chemotherapy/radiation/disseminated cancer, bleeding disorder, anemia, preoperative sepsis/SIRS, wound class, discharge to non-home location, open surgery, blood transfusion, and pre-discharge major complications. Medical complication model also adjusted for age, diabetes, ASA class, pulmonary comorbidity, cardiac comorbidity, bleeding disorder, anemia, open surgery, discharge to a non-home location, and pre-discharge major complications. Pain model also adjusted for age, race, diabetes, ASA class, anemia, open surgery, discharge to a non-home location, and blood transfusion.  Adjusted Readmission Hazard Ratios (95% CI) 1-3 days LOS (top line): Reference 4-5 days LOS (2nd line from top): 1.28 (1.14, 1.44) p-value<0.001 6-7 days LOS (3rd line from top): 1.58 (1.40, 1.80) p-value<0.001 8+ days LOS (Bottom line): 1.70 (1.49, 1.93) p-value<0.001 Logrank test: p-value<0.001 Breslow test: p-value<0.001 LOS: Postoperative length of stay Model adjusted for age, race, transfer status, body mass index, diabetes, ASA class, functional status, smoking, pulmonary comorbidity, hepatic insufficiency, cardiac comorbidity, renal insufficiency, neurological comorbidity, chemotherapy, radiation, disseminated cancer, bleeding disorder, chronic steroid use, preoperative sepsis, preoperative transfusion, anemia, wound class, discharge location, open surgery, emergency case status, and pre-discharge complications.
Back to 2014 Annual Meeting Abstracts
|