|
Back to Annual Meeting Posters
Surgical Apgar Score Does Not Predict Morbidity and Mortality for Patients Undergoing Pancreaticoduodenectomy for Pancreatic Adenocarcinoma
Paul Toomey*, Sharona B. Ross, Charles Tkach, Nicholas J. Sarabalis, Kenneth Luberice, Kaulin Jani, Alexander Rosemurgy
General Surgery, Florida Hospital Tampa, Tampa, FL
Introduction: The Surgical APGAR was published in 2007 as a simple method for predicting postoperative morbidity and mortality for patients undergoing General Surgery operations. The Surgical APGAR consists of three objective measures of an individual's intraoperative course: the lowest heart rate, the lowest mean arterial blood pressure (MAP), and the estimated blood loss (EBL). The Surgical APGAR was shown to predict major morbidities for patients undergoing pancreaticoduodenectomy; the purpose of this study was to validate that the Surgical APGAR predicts major morbidity and mortality for patients undergoing pancreaticoduodenectomy for pancreatic adenocarcinoma.
METHODS: Patients who underwent pancreaticoduodenectomy for pancreatic adenocarcinoma from 1991-2012 are prospectively followed. Anesthesia records were reviewed and the lowest heart rate, lowest MAP, and the EBL of the operations were recorded. The Surgical APGAR scores were calculated using the proposed algorithm. Major morbidities were classified using Clavien scores and the in-hospital mortality was assessed. Data are presented as median, mean ± standard deviation. Correlations were calculated using logistic regression analysis and p-values < 0.05 were considered significant.
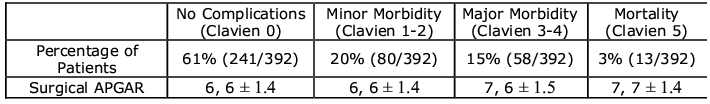
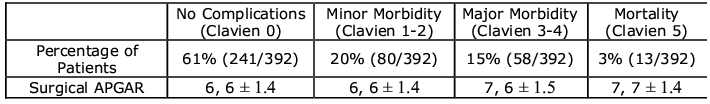
RESULTS: 392 patients underwent pancreaticoduodenectomy for pancreatic adenocarcinoma. The median lowest heart rate was 64, 64 ± 10.5, the median lowest MAP was 64 mmHg, 63 mmHg ± 7.9, the estimated blood loss was 500 bpm, 650 bpm ± 601.3, and the Surgical APGAR was 6, 6 ± 1.4. The lowest heart rate, lowest MAP, or EBL did not independently or in combination correlate with Clavien scores. There was no correlation between Surgical APGAR and Clavien scores (Table: p=NS) or mortality.
CONCLUSIONS: Pancreatic cancer is the fourth leading cause of cancer death in the United States and has the highest fatality rate. Complications with pancreaticoduodenectomy for pancreatic adenocarcinoma remain high and contribute to poor survival. Scoring systems to predict complications after surgical intervention have been developed but have been cumbersome to calculate, inaccurate, and impractical. The introduction of the uniquely simple Surgical APGAR provided hope for a practical prospective predictor of complications and early mortality for patients undergoing surgical operations. The Surgical APGAR was initially found to correlate with major complications following pancreaticoduodenectomy; however, this study refutes these findings. Herein, we show that the Surgical APGAR does not predict major morbidity or mortality for patients undergoing pancreaticoduodenectomy for pancreatic adenocarcinoma. Still, intuitively, patients benefit from short operations without hemodynamic instability and blood loss or transfusions.
Back to Annual Meeting Posters
|