|
Back to Annual Meeting Posters
Impact of Margin Clearance on Survival After Pancreaticoduodenectomy for Pancreatic Ductal Adenocarcinoma: What Is a "True" Negative Margin?
Yasushi Hashimoto*, Yoshiaki Murakami, Kenichiro Uemura, Takeshi Sudo, Naru Kondo, Taijiro Sueda
Department of Surgery, Applied Life Sciences Institute of Biomedical & Health Sciences, Hiroshima University, Hiroshima, Japan
BACKGROUND: Microscopic involvement of a resection margin by tumor is associated with a poor prognosis. It is unclear whether a proximity to resection margins by tumor confers a survival benefit over margin involved R1 resection of their pancreatic ductal adenocarcinoma (PDAC) after pancreticoduodenectomy (PD). The aim is to better understand the impact of resection status on clinical and pathologic staging, and long-term survival after PD for PDAC, and to explore the prognostic significance of a proximity to surgical margins.
METHODS: We assessed the relationships between margin involvement (R1), the proximity to resection margins (R0-close) and outcome in a cohort of 124 consecutive patients who underwent PD for PDAC between 2002 and 2012. Resected specimens were analyzed according to the improved standardized pathology protocol which included permanent section analysis of the surgical margins. R0-close margin was defined as tumor within 1-mm of the resection margins and a patient with a margin of greater than 1-mm was defined as R0-wide margin. Follow-up data on overall and disease-free survival, presence and site of tumor recurrence were examined.
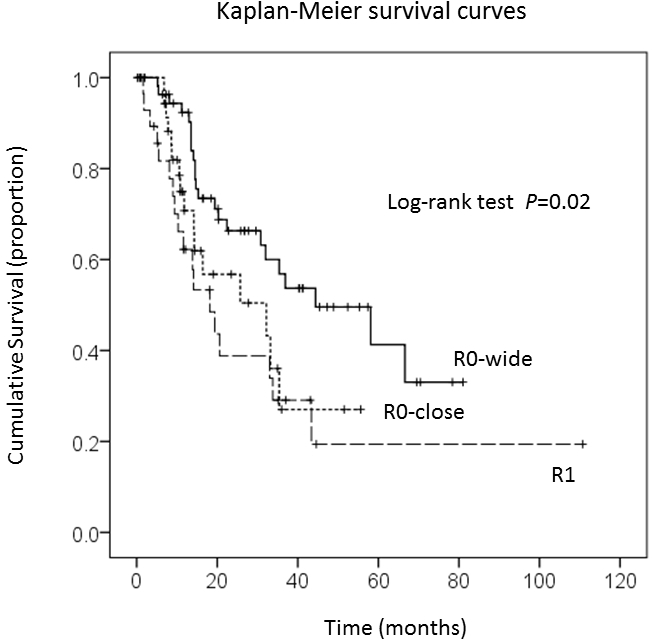
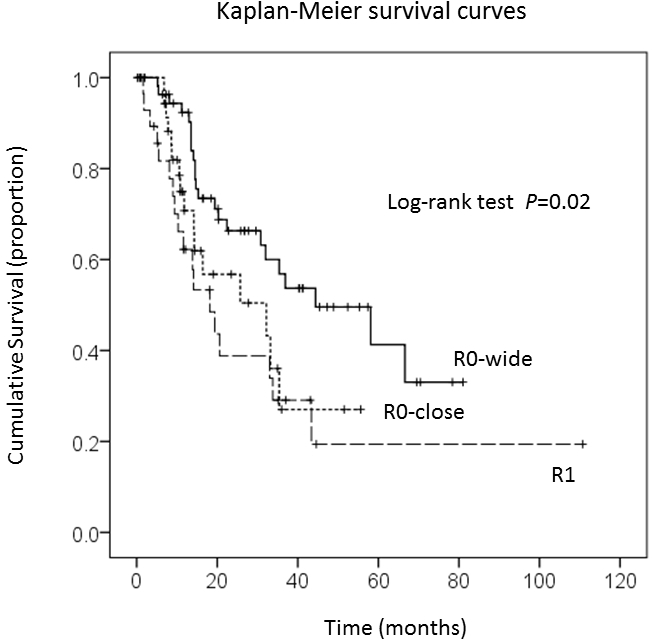
RESULTS: Of the 124 patients, the resection margins were positive (R1) in 30 (24%) and negative (R0) in 94 patients (76%) including 38 patients (31%) with an R0-close resection. Patients with R1 resections had an unfavorable survival compared with those with R0 resections (median, 18 vs 35 months; P<0.01), but survival with R0-close margin were comparable to R1 resections: but both groups had a significantly shorter survival than patients with R0-wide margins (18 vs 32 vs 44 months, respectively; P=0.02). Disease-free survival was shorter in R1/R0-close margins comparing to R0-wide group (median, 12 vs 19 months; P=0.04). By multivariate analysis, predictors of R1/R0-close margins were patients underwent portal vein resection and larger tumor size of greater than 20-mm. The pattern of tumor recurrence had a greater rate of regional metastases in the R1/R0-close margins group comparing to patients with R0-wide margins (48% vs 14%; P=0.01).
CONCLUSIONS: These data demonstrate that a margin clearance of more than 1-mm is important for long-term survival in a subgroup of patients. Complete histologic evaluation of the resected PD specimens is important for prognosis in patients with PDAC who underwent PD. More aggressive therapeutic approaches that target locoregional disease such as neoadjuvant radiation therapy may be beneficial in patients with close surgical margins.
Back to Annual Meeting Posters
|