|
Back to Annual Meeting Posters
Weight-Loss Interventions for Morbidly Obese Patients With Compensated Cirrhosis: a Markov Decision Analysis Model
Bianca Bromberger*1, Kristoffel Dumon2, Rashikh a. Choudhury1, Paige Porrett2, Kenric Murayama2
1Perelman School of Medicine at the University of Pennsylvania, Philadelphia, PA; 2Department of Surgery, University of Pennsylvania Health System, Philadelphia, PA
PURPOSE: With the rising prevalence of obesity, nonalcoholic steatohepatitis is an increasingly common cause of cirrhosis and indication for liver transplantation. However, since many centers require that patients maintain a BMI <40 kg/m2 to be eligible for transplantation, many morbidly obese patients are excluded from this life-saving therapy. It is currently unknown which weight loss interventions should be utilized in morbidly obese cirrhotic patients in order to improve transplantation candidacy. This study therefore aimed to compare the efficacy of three methods of weight loss in morbidly obese patients with compensated cirrhosis [Roux-en-Y gastric bypass (RYGB), Adjustable Gastric Banding (AGB), and one year of diet and exercise]. We hypothesized that the faster and more significant weight loss achieved by RYGB would increase life expectancy.
METHODS: A Markov state transition model was developed to assess the survival benefit of undergoing RYGB, AGB or one year of diet and exercise in morbidly obese patients with compensated cirrhosis. The model assumed that a BMI <40 kg/m2 was required for patients to be listed for transplantation. State transition values were obtained from the literature in order to best estimate the rates of weight loss, progression of disease, wait-listing and transplantation. The model was analyzed using decision analysis software (TreeAge Pro 2012). Base-case and sensitivity analyses of pre-intervention BMI and peri-operative mortality were performed.
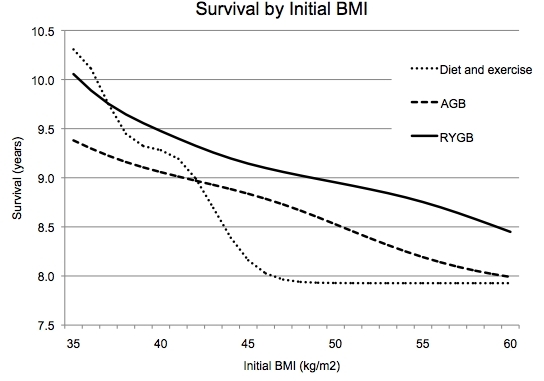
RESULTS: The base case analysis of a 45 year-old patient with compensated cirrhosis, a BMI of 45 kg/m2 and no weight-loss intervention revealed an average survival of 7.93 years. Patients transitioned into lower weight classes fastest in the RYGB simulation. The average survival for the weight loss simulations were 9.14, 8.84, and 8.16 years for RYGB, AGB, and diet and exercise, respectively. Sensitivity analysis of initial BMI revealed that RYGB increased life expectancy compared to AGB in all patients that were severely or morbidly obese (all BMIs greater than 35 kg/m2) and in all patients with a BMI greater that 36.98 kg/m2
compared to one year diet and exercise.
CONCLUSION: In morbidly obese patients with compensated cirrhosis, RYGB is the most effective means to decrease BMI. Importantly, this intervention leads to increased life expectancy in this population, potentially because of improved access to liver transplantation and/or impact on disease progression.
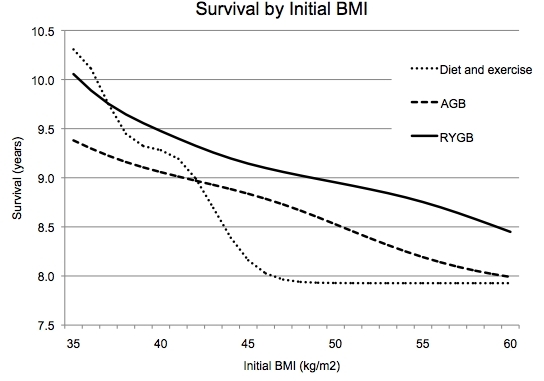
Sensitivity analysis of survival post-weight loss intervention based on initial BMI
Back to Annual Meeting Posters
|