|
Back to Annual Meeting Posters
Toward Improved Staging of Esophageal Adenocarcinoma in the Era of Neoadjuvant Chemotherapy; Lymph Node Harvest and Lymph Node Positivity Ratio Provide Better Survival Models
Dylan R. Nieman*, Michal J. Lada, Michelle S. Han, Poochong Timratana, Christian G. Peyre, Carolyn E. Jones, Thomas J. Watson, Jeffrey H. Peters
Department of Surgery, University of Rochester, Rochester, NY
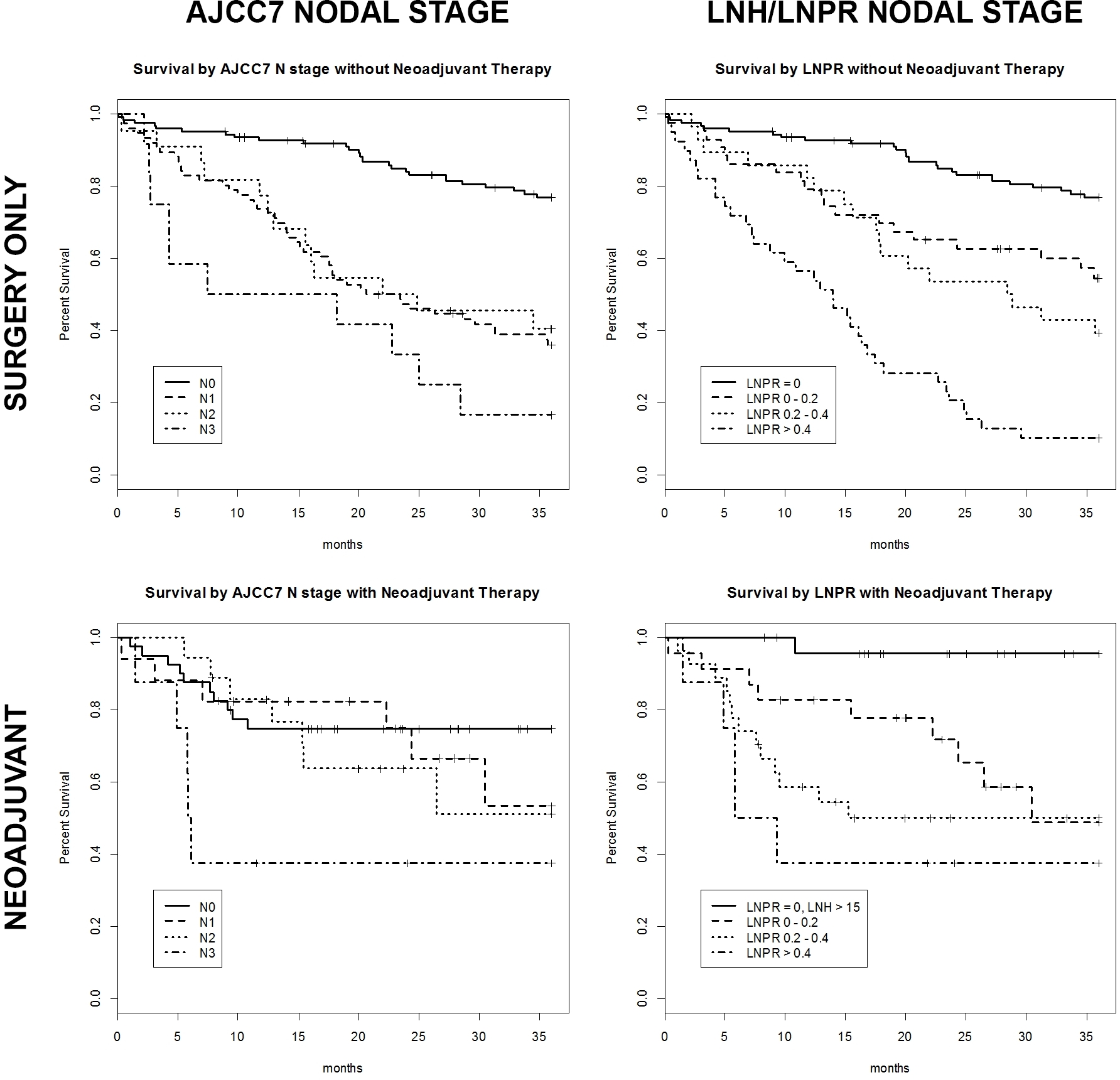
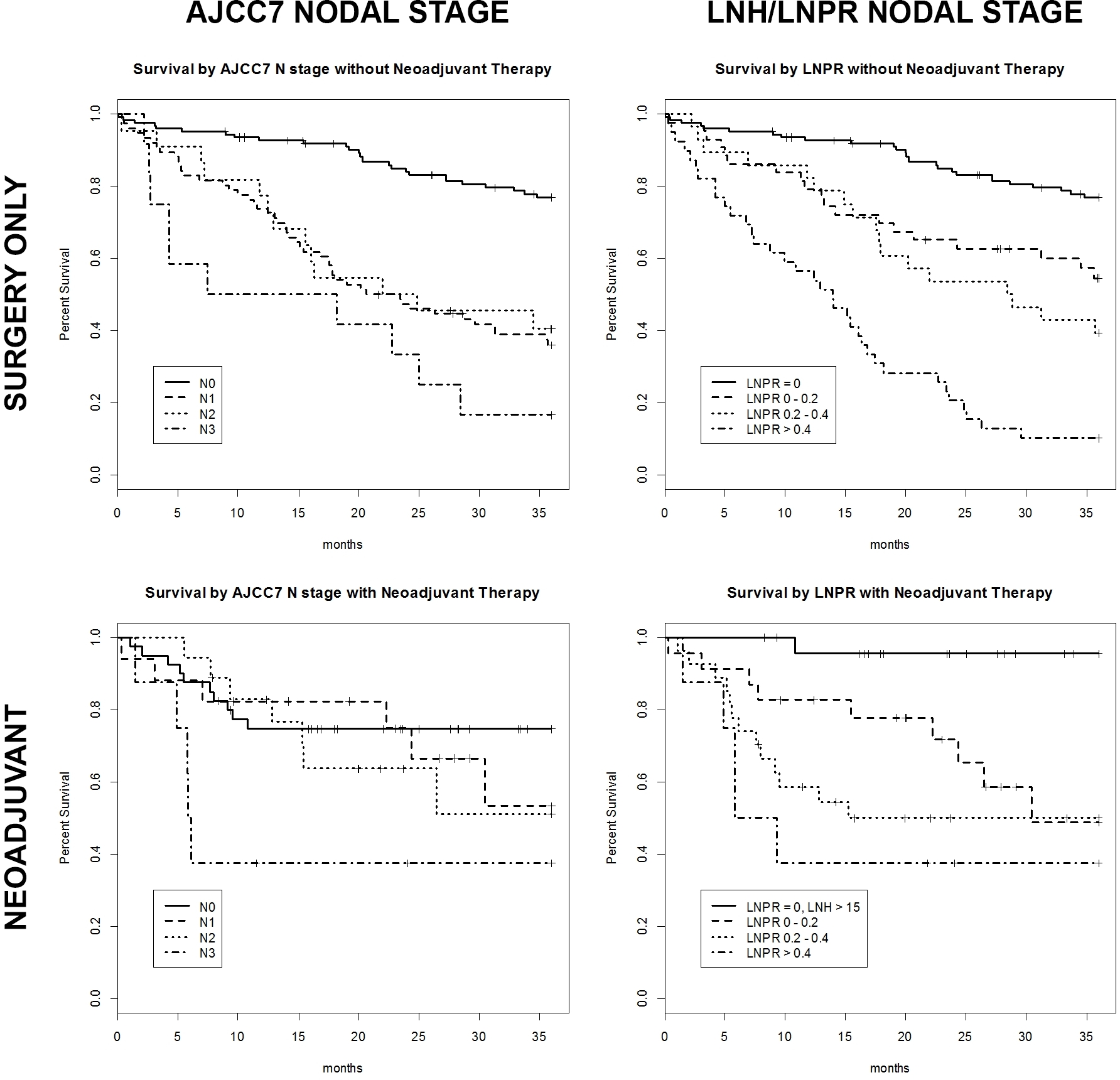
INTRODUCTION: As pre-operative chemoradiation followed by esophagectomy has become standard therapy in patients with resectable esophageal adenocarcinoma (EAC), traditional pathological staging has become a less useful prognostic tool. The 7th edition of the American Joint Commission on Cancer (AJCC7) staging system for EAC is derived from data on patients undergoing esophagectomy without neoadjuvant therapy and classifies lymph node status by the number of involved lymph nodes. Lymph node harvest (LNH) and lymph node positivity ratio (LNPR) have been suggested to be prognostic indicators but have not found widespread support. In an effort to develop a valid staging model in the era of neoadjuvant therapy, we compared the predictive value of LNH and LNPR to AJCC7 staging in a large cohort of patients undergoing resection for EAC.
METHODS: The study population consisted of 316 patients who underwent R0 esophagectomy for EAC from 1/00 to 12/11 (86% male; mean age 64.0±10.3 years). Survival functions were estimated using the Kaplan-Meier method. Classification thresholds for both LNPR and LNH were derived by recursive partitioning using conditional inference trees comparing survival functions. Based on these analyses, LNPR was stratified and Cox proportional hazards regression models were used to compare predictive value of lymph node categorization strata.
RESULTS: Median lymph node harvest was 12 (IQR 7-20). 51% of patients were N0, 29% N1, 13% N2. Median overall survival was 63.4 months (95%CI 40.6 - 92.3) and 5-year overall survival was 50.7% (95%CI 45.0 - 57.2). Eighty-three patients (26%) received neoadjuvant chemotherapy, radiation therapy or both. In patients who received neoadjuvant therapy and had no lymph node metastasis identified (40/83; 48%), recursive partitioning analysis yielded a LNH threshold of 15 for discrimination of survival functions. LNH ≥ 15 was associated with a significant survival advantage (3-year survival 95 vs. 38%; p = 0.000022). Similarly, recursive partitioning analysis yielded LNPR categories of less than 20%, 20-40%, or greater than 40% as significantly discriminant of survival functions. In patients who received neoadjuvant therapy, LNPR was more predictive of survival than number of positive lymph nodes as categorized by AJCC7 (p=0.00018 vs. 0.033). In the 256 patients who received no neoadjuvant therapy, LNH was not a significant predictor of survival after node negative resection, although LNPR was a stronger predictor of survival than the current nodal staging system (p-value 0.000015 vs. 0.05).
CONCLUSION: For patients receiving neoadjuvant therapy, both LNH and LNPR are more predictive of survival than the number of lymph node metastases detected in esophagectomy specimens. A minimum LNH of 15 is necessary to establish reliable N0 staging in this cohort.
Back to Annual Meeting Posters
|