|
Back to Annual Meeting Posters
Jackhammer Esophagus in High Resolution Manometry: Clinical Features and Surgical Implications
Michal J. Lada*, Dylan R. Nieman, Michelle S. Han, Poochong Timratana, Christian G. Peyre, Carolyn E. Jones, Thomas J. Watson, Jeffrey H. Peters
University of Rochester Medical Center, Rochester, NY
Introduction: The clinical significance of Jackhammer Esophagus, an uncommon esophageal motility disorder characterized by repetitive high amplitude esophageal contractions, is unclear. It has been increasingly identified since the introduction of High Resolution Manometry. This study assessed the clinical features and surgical implications of a diagnosis of Jackhammer Esophagus (JE) via High Resolution Manometry (HRM).
Methods: The clinical records and HRM data of 1216 consecutive patients undergoing HRM between 12/2009 and 9/2012 were reviewed. Patients with previous foregut surgery, classic achalasia and distal esophageal spasm were excluded. Jackhammer esophagus was defined according to the most recent Chicago Classification as ≥1 swallow with distal contractile integral (DCI) >8000mmHg*cm*s. HRM variables were compared with 35 normal volunteers via Mann-Whitney U-Test for non-parametric univariate analysis.
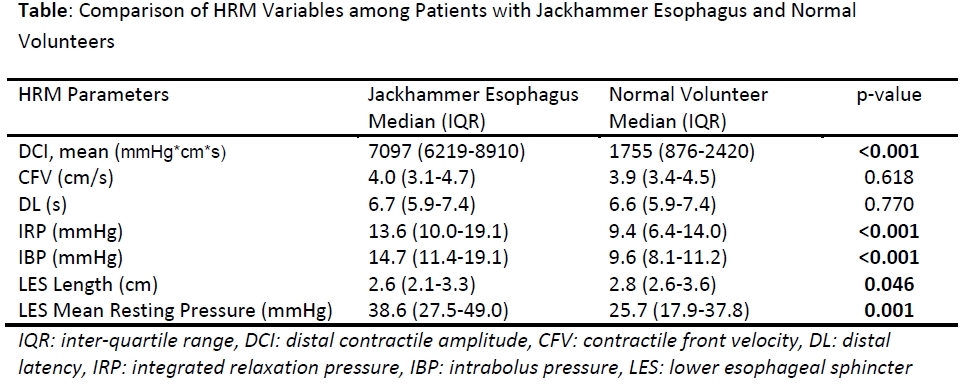
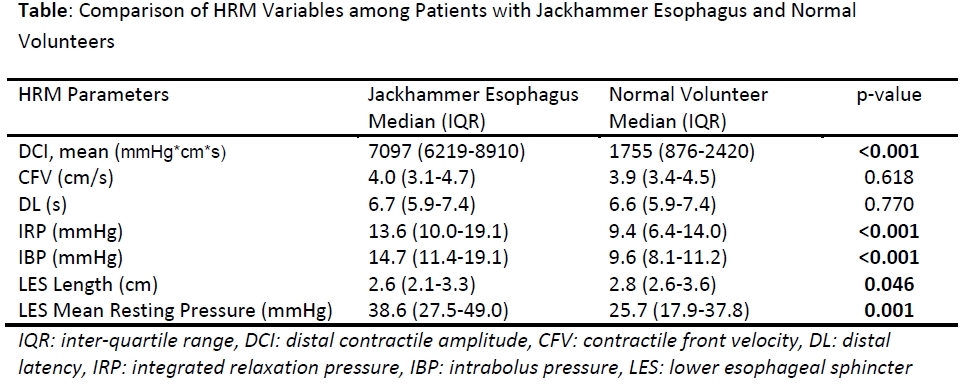
Results: Forty-two patients (3.5%) met HRM criteria for JE, 71% were female with a mean age 59.0+/- 11.8 years. The most common presenting symptoms were chest pain (30%), heartburn (14%) and dysphagia (14%). Other less common symptoms included regurgitation, abdominal pain, nausea, cough and shortness of breath. Compared with 35 healthy volunteers, patients with JE not only had significantly elevated DCI, but also higher mean lower esophageal sphincter resting pressure, intrabolus pressure and integrated relaxation pressure (IRP), (Table). The median number of individual swallows with DCI >8000mmHg*cm*s per patient was 3.5 (IQR 2.0-6.0). Overall, the IRP was normal in 23 (55%) and elevated in 19 (45%). An elevated IRP and/or positive pH study, suggestive of JE being a secondary motility disorder, was present in 27 of 42 patients. Hiatal Hernia (HH), identified endoscopically, was present in 18 patients (43%). Abnormal esophageal acid exposure was found in 12 patients of whom 4 had elevated IRP (range 18.2-19.8). Of the 33 patients treated medically, 30 were trialed on combinations of calcium channel blockers (CCB), nitrates or proton-pump inhibitors (PPI) and 3 received Botox. Eight patients underwent Nissen Fundoplication +/- hiatal hernia repair and 1 patient underwent a distal myotomy. Complete resolution of chest pain or heartburn was encountered in all post-surgical patients, with a median follow-up of 20 days (range 14-364).
Conclusions: Jackhammer esophagus is an uncommon motility disorder diagnosed in 3.5% of patients with esophageal symptoms. Afflicted patients are predominantly female and present with chest pain, likely owing to the intensity of the esophageal contractions. Patients with isolated JE are managed medically with a constellation of agents including CCBs and nitrates. For patients with JE and concomitant reflux or hiatal hernia, Nissen Fundoplication is an effective treatment regardless of the motility findings.
Back to Annual Meeting Posters
|