|
Back to Annual Meeting Posters
Pneumoperitoneum Following Abdominal Surgery; Can We Distinguish Benign vs. Problematic?
I. Michael Leitman*1, Marissa M. Montgomery1, Joseph E. Sabat1, Laura Bernstein1, Burton Surick1, Barbara Zeifer2, Hristina Natcheva2, Franklin Nwoke2, Charles S. Holland1, Anthony Sorrentino1
1Surgery, Albert Einsteil College of Medicine-Beth Israel Medical Center, New York, NY; 2Radiology, Albert Einstein College of Medicine-Beth Israel Medical Cener, New Yotk, NY
INTRODUCTION
Pneumoperitoneum seen on postoperative imaging presents a diagnostic dilemma. It can be a normal finding secondary to air that was introduced at surgery, which typically resolves in a matter of days. On the other hand, it could also represent a sign of a perforated viscus or an anastomotic leak, which might require re-operation. Distinguishing one from the other is critical to successful management. This study examines clinical and radiological findings in order to determine which are able to facilitate the distinction of benign versus pathological postoperative pneumoperitoneum.
METHODS
A retrospective analysis of medical records from a large urban teaching hospital was performed. Imaging studies reporting "pneumoperitoneum," "free air," and "free intraperitoneal air," from July 2006 through June 2012 were selected for review. The cases were divided into three groups: patients who ultimately were returned to the operating room and had findings requiring operative intervention, those who were returned to surgery but did not have evidence of pathology requiring operative intervention, and those who were managed expectantly. Demographic, physical findings and laboratory studies were recorded. The radiological studies were reviewed in an attempt to quantify the amount of free intra-peritoneal air.
RESULTS
68 patients were found to have postoperative pneumoperitoneum after abdominal surgery. Twenty patients (29%) underwent re-exploration because of presumed intra-abdominal complication and the remainder of patients were managed by observation alone. Nine patients had prior open surgery and 11 had minimally invasive abdominal procedures. At surgery, 14 patients (70%) were found to have pathologic conditions requiring intervention. The other six were explored but were found to have conditions that could have been managed without re-exploration. The patients in each group were similar with regard to age, gender vital signs, pain score, physical findings, amount of free air or open vs. laparoscopic procedure. However, patients requiring re-operation were found to have pneumoperitoneum 5.7 days after initial surgery compared to postoperative 2.7 days for those that could be managed expectantly (P = 0.004). 15% of the patients undergoing re-operation died compared to 19% who were managed without surgery (P > 0.05), none of which were related to intra-abdominal pathology. None of the other variables were found to be significantly different between groups.
CONCLUSIONS
This study suggests that patients with postoperative free air still present a diagnostic and therapeutic challenge. However, free air several days following surgery may provide an indication that this finding should be of greater concern. Such patients have a greater likelihood of requiring reoperation for the treatment of a postoperative complication.
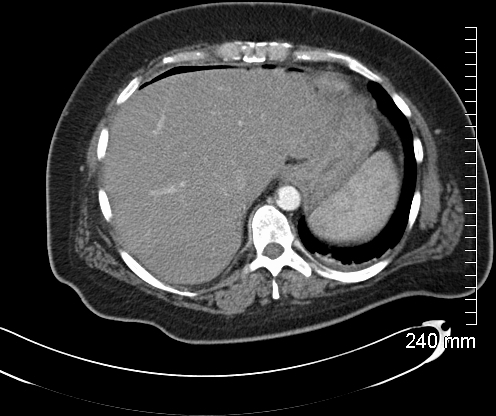
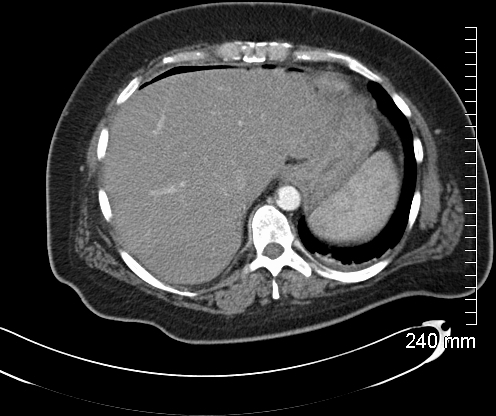
CT scan with contrast on sixth postoperative day following laparoscopic sleeve resection demonstrating free air over the liver and around spleen
Back to Annual Meeting Posters
|