|
Back to Annual Meeting Posters
Trends in the Management of Acute Cholecystitis: Prevalence of Percutaneous Cholecystostomy and Delayed Cholecystectomy in an Elderly Population
John D. Cull*2, Dahlia Rice2, Alexander J. Czubak1, Eric C. Brown1, Jose M. Velasco1,2
1Surgery, NorthShore University HealthSystem, Skokie, IL; 2Surgery, Rush University Medical Center, Chicago, IL
Background: Management of patients with acute cholecystitis (AC) remains controversial. Published guidelines recommend early laparoscopic cholecystectomy (LC) as the preferred treatment option. Percutaneous cholecystostomy tubes (PCT) had been primarily used in the setting of patients with serious comorbidities, severe cholecystitis in the elderly, and in cases where LC can be technically challenging. We reviewed our experience in the management of AC in the elderly to identify factors that could influence outcomes; specifically, the prevalence of PCT, the timing of cholecystectomy, and adherence to published guidelines in their management.
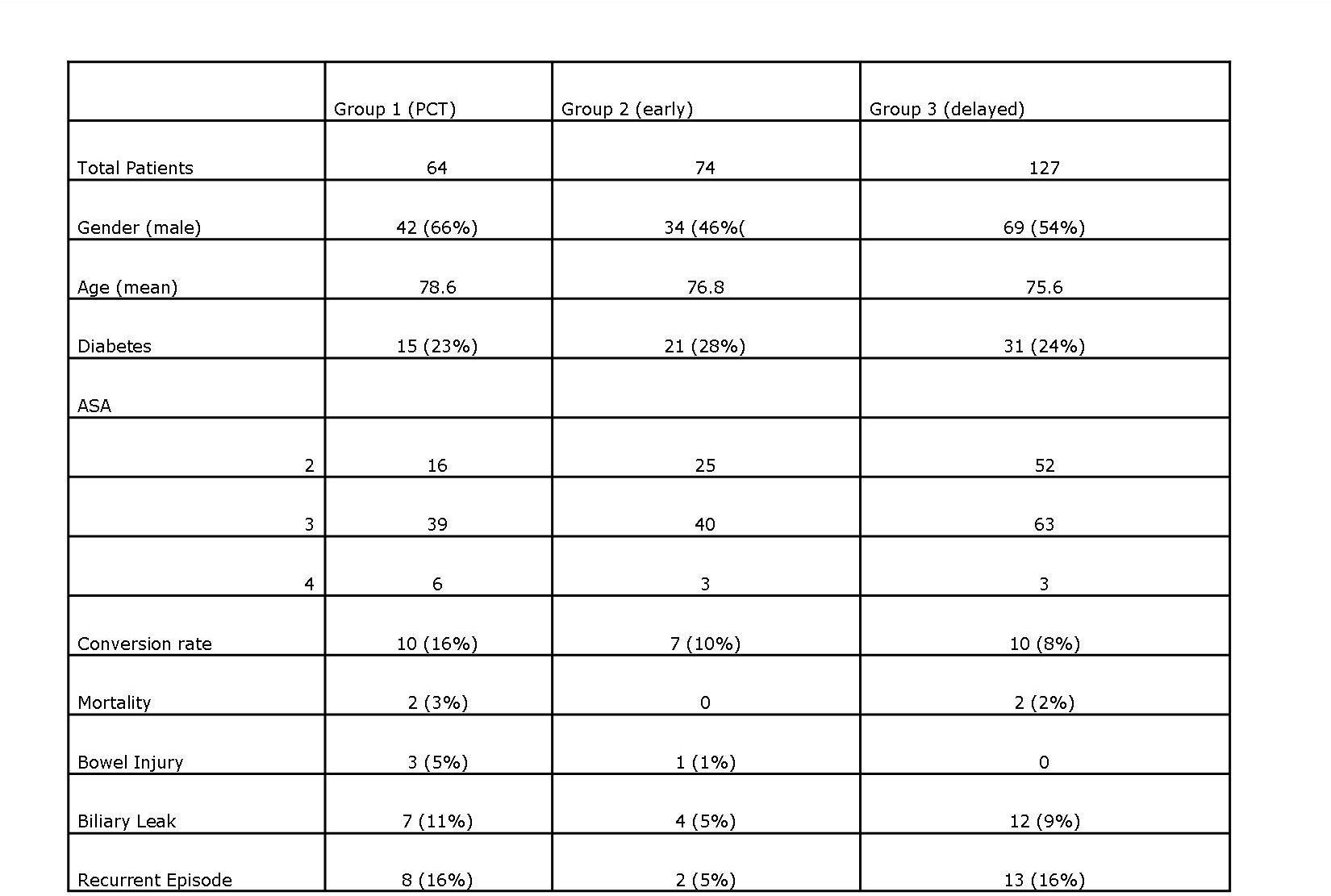
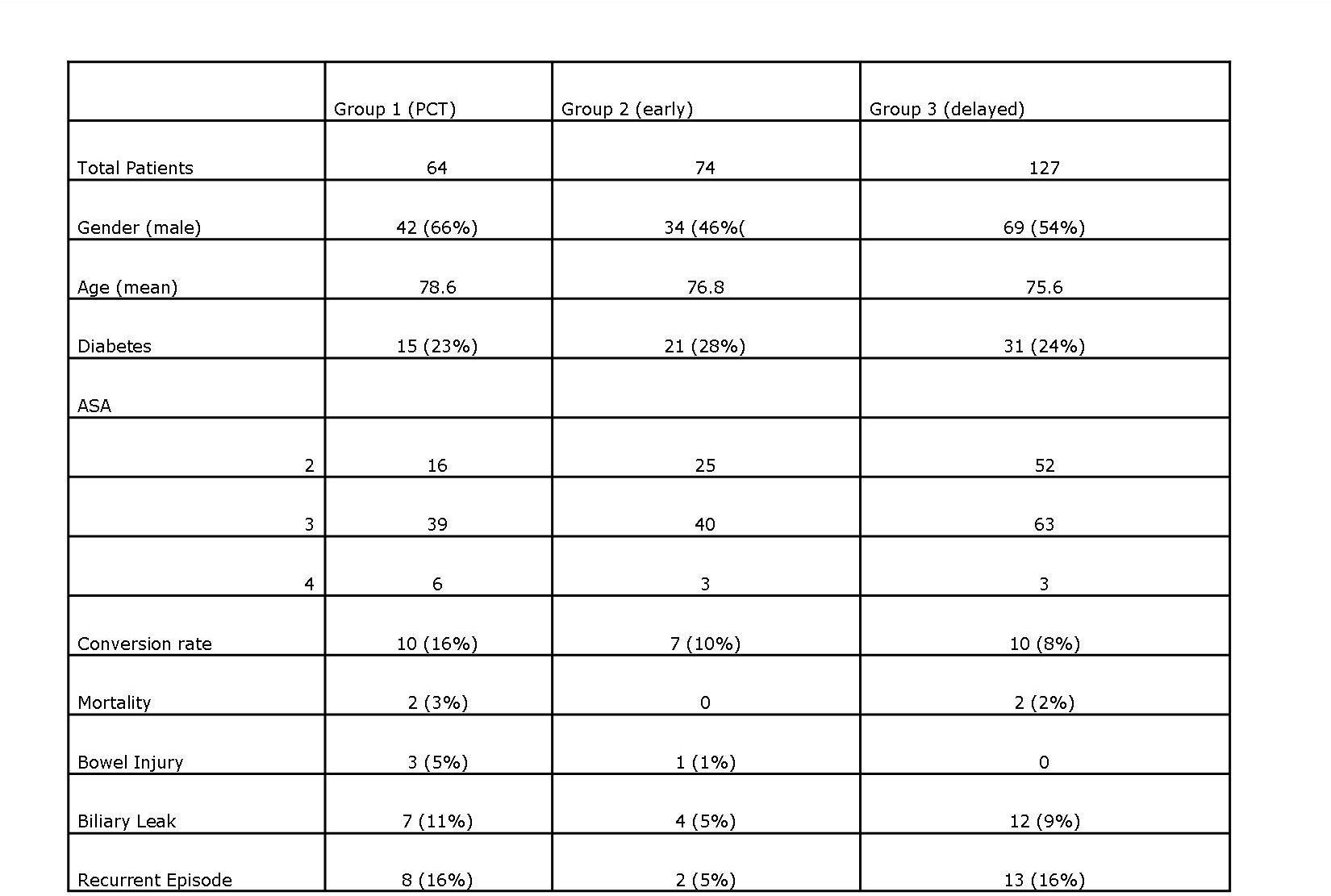
Methods: A retrospective review of 806 elderly patients (>65) with the primary diagnosis of biliary disease was performed from 2009 through 2011. ICD-9 codes were used. Patients were divided into three groups: PCT (Group 1), early cholecystectomy (Group 2), and late cholecystectomy (Group 3). All three groups were compared with respect to outcome measures and covariates. Logistic regression and Fisher exact test were used to determine statistical significance.
Results: We reviewed 265 patients with a histologic diagnosis of AC. Out of 75 patients who initially had PCT, 64 (24%) underwent interval cholecystectomy, 74 (28%) early cholecystectomy, and 127 (48%) delayed cholecystectomy. The mean age of patients was 77 with no statistical difference among groups. Patients in Group 1 were more likely to have ASA scores of 4 when compared to those in Groups 2 and 3 (p =0.04). After removing those with an ASA of 4, no significant difference existed among the three groups with regard to covariates. Regarding outcomes, there was no difference in conversion rates, biliary leak, bowel injury, need for reoperation, or 30 days mortality among the three groups. Overall conversion rate in the three groups was 11% with no statistical significance between groups. Compared to Group 2, patients in Group 1 were five times more likely (p =0.04) and those in Group 3 were four times more likely (p =0.06) to have a recurrent episode of pancreatitis, cholecystitis and/or cholangitis from the time of diagnosis until operation.
Conclusion: Despite guidelines recommending early cholecystectomy, patients in our study were more likely to have their cholecystectomy delayed after a course of antibiotics or PCT (24%). Patients undergoing PCT placement or delayed cholecystectomy did not have a lower conversion rate when compared to those who underwent early cholecystectomy, and they were more likely to have recurrent episodes of AC/pancreatitis or cholangitis. Based on our review, patients who are medically fit for an operation should undergo early cholecystectomy since interval cholecystectomy is not associated with better outcomes. Future studies will be aimed at looking at resource utilization and overall cost in these patients.
Back to Annual Meeting Posters
|