|
Back to Annual Meeting Program
Hospital Center Effect for Laparoscopic Colectomy Among Elderly Stage I-III Colon Cancer Patients
Zhiyuan Zheng2, Nader Hanna*1, Eberechukwu Onukwugha2, Kaloyan a. Bikov2, C. Daniel Mullins2
1Surgery, University of Maryland School of Medicine, Baltimore, MD; 2Pharmaceutical Health Services Research Department, University of Maryland School of medicine, Baltimore, MD
Objective
To investigate hospital level variation in short-term laparoscopic colectomy outcomes among stage I-III elderly colon cancer patients.
Background
Surgical outcomes are associated with patient and surgeon characteristics. If outcomes are also impacted by the specific hospital where the surgery occurs, there is a hospital center effect (HCE). Previous studies of laparoscopic colectomies focus on patient, provider and hospital characteristics, ignoring potential HCE.
Methods
The Surveillance, Epidemiology and End Results (SEER)-Medicare dataset was used to identify stage I-III colon cancer patients in 2003 to 2007 with laparoscopic colectomies. Multilevel model regressions were utilized to study potential HCE for length of stay (LOS), 30-day re-hospitalization, and in-hospital mortality, adjusting for patient, surgeon and hospital level characteristics. To quantify the impact of HCE, we calculated median instantaneous rate ratio (MIRR) for LOS and median odds ratio (MOR) for in-hospital mortality and 30-day re-hospitalization. Sensitivity analyses were also conducted for high volume/medical school affiliated hospitals and colorectal surgeons.
Results
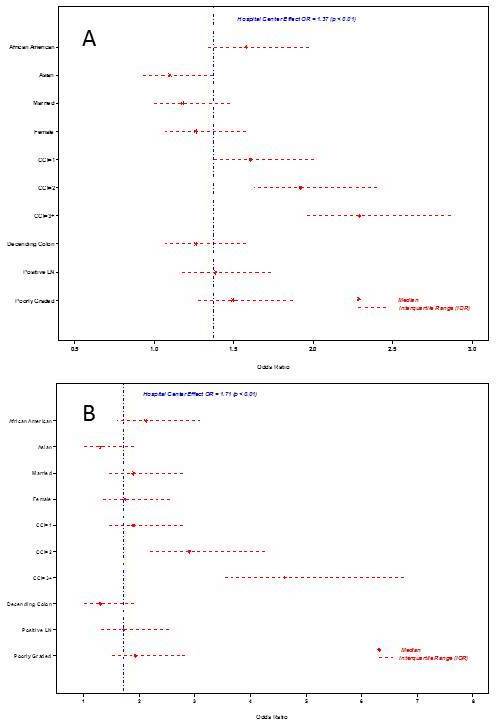
The multilevel analyses based on 4,617 patients from 465 hospitals documented significant HCEs for LOS (MIRR = 1.36; p < .001) and in-hospital mortality (MOR = 1.72; p = 0.037), but no HCE for 30-day re-hospitalization. For patients with CCI = 3+, MIRR rose to 2.27 for LOS and MOR rose to 6.87 for in-hospital mortality. The sensitivity analyses confirmed our findings. HCE was significant for LOS in all subgroup analyses, and was significant for in-hospital mortality for high volume/medical school affiliated hospitals.
Conclusion
HCE is an important source of variation for laparoscopic colectomy short-term outcomes, and it is still significant when patient, provider and hospital level characteristics are adjusted. HEC exists for both LOS and in-hospital mortality. The findings are robust to high volume/medical school affiliated hospitals and colorectal surgeons. HCE is a potential area to improve the quality of care for stage I-III laparoscopic colon cancer patients.
Subgroup analyses for hospital center effect on short-term outcomes of laparoscopic colectomy
| High Volume Hospitals (>=30) | ColorectalSurgeons | Affiliated with Medical School | Not Affiliated with Medical School | | N of Hospitals | 43 | 119 | 196* | 281 | | N of Patients | 1661 | 1020 | 2397 | 2220 | | MIRR for LOS (P-value) | 1.24 (<0.001) | 1.62 (<0.001) | 1.21 (<0.001) | 1.46 (<0.001) | | MOR for In-hospital Mortality (P-value) | 1.96 (0.004) | NA | 2.09 (0.022) | 1.63 (0.132) |
* There are 12 hospitals who changed their medical school affiliation during the study period. Therefore, these hospitals appeared in both affiliated and not affiliated with medical schools.
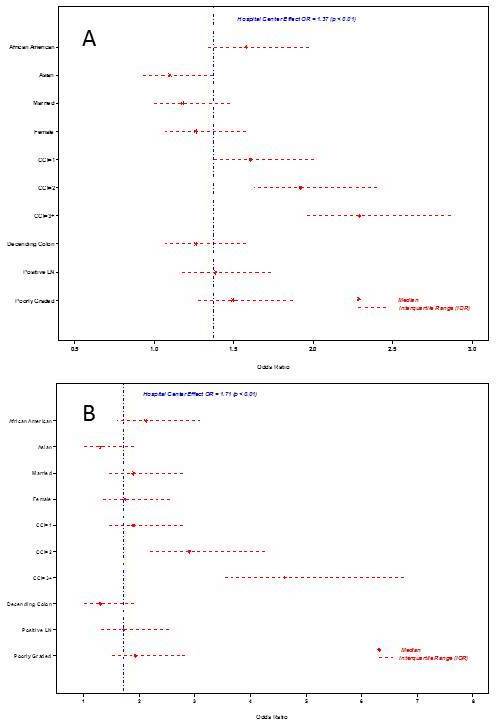
Joint impact of HCE and selected patient level characteristics on LOS (A) and in-hospital mortality (B)
Back to Annual Meeting Program
|