|
 |
Back to Annual Meeting Program
Morbidity and Mortality After Pancreaticoduodenectomy in Patients With Borderline Resectable Type C Clinical Classification
Ching-Wei D. Tzeng1, Matthew Katz1, Jason B. Fleming1, Holly M. Holmes3, Jeffrey E. Lee1, Peter W. Pisters1, Jean-Nicolas Vauthey1, Gauri R. Varadhachary2, Robert A. Wolff2, James Abbruzzese2, Thomas Aloia1
1Dept of Surgical Oncology, The Univ. of Texas MD Anderson Cancer Center, Houston, TX; 2Dept of GI Medical Oncology, The Univ. of Texas MD Anderson Cancer Center, Houston, TX; 3Dept of General Internal Medicine, The Univ. of Texas MD Anderson Cancer Center, Houston, TX
Background: We previously described the clinical classification of patients with resectable pancreatic tumor anatomy but marginal performance status (PS) or reversible comorbidities as "borderline resectable type C" (BR-C for condition/comorbidity). This study was designed to analyze the nationwide incidence and risk factors for post-pancreaticoduodenectomy (PD) morbidity/mortality in patients who could be classified as BR-C.
Methods: All elective PDs were evaluated in the 2005-10 ACS-NSQIP database. BR-C was defined by the following: age≥80, lack of independent function, pulmonary disease, ascites/varices, recent myocardial infarction/angina, stroke history, steroid use, weight loss>10%, and/or preoperative sepsis. Clinical variables potentially associated with 30-day morbidity/mortality were analyzed, with a focus on the development of postoperative major complications defined as: pneumonia, re-intubation/ventilation>48hr, renal failure, cardiovascular event, sepsis, re-operation, dehiscence, organ space infection, and venous thromboembolism.
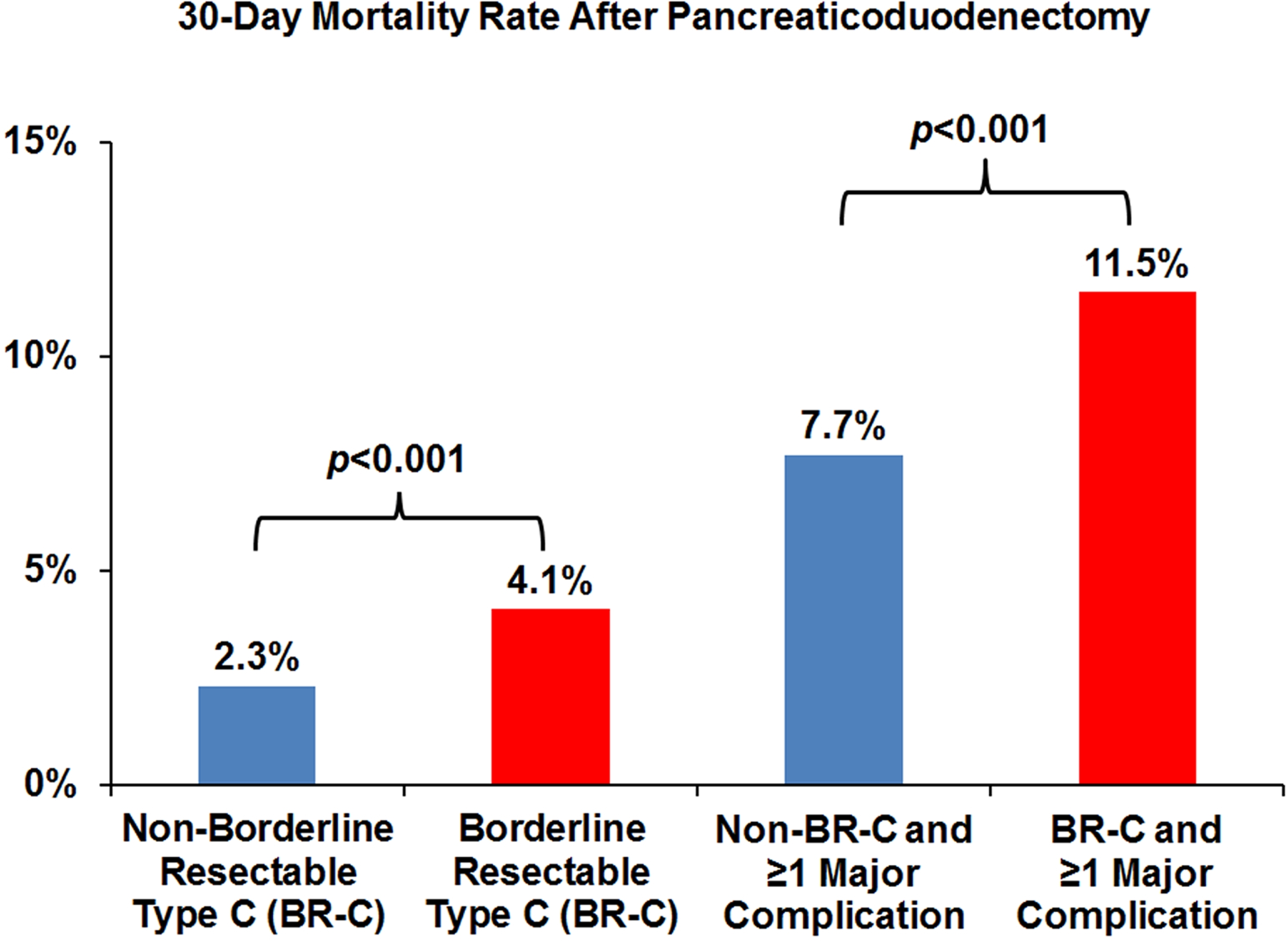
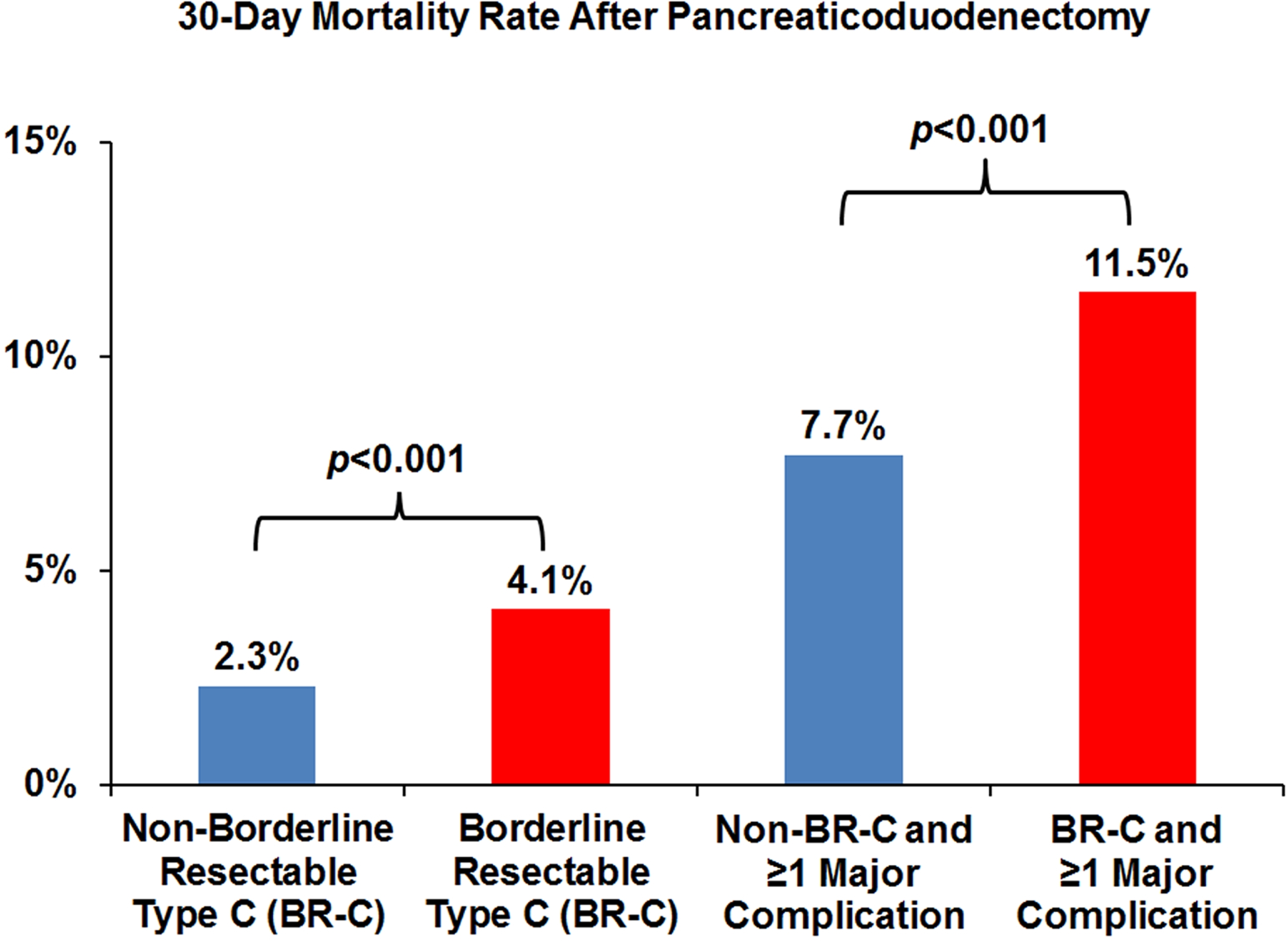
Results: Of 8,266 PDs, 3,033 (36.7%) involved patients with BR-C classification. Analysis of preoperative variables determined that BR-C patients were more likely to have abnormal preoperative lab values (albumin, liver function tests, leukocytosis, coagulation, hematocrit, uremia, creatinine, all p≤0.002) and need for preoperative hospitalization (23.6% vs. 12.3%, p<0.001). Despite similar operative times (≥360min in 47.2% BR-C vs. 49.2% non-BR-C, p=0.081), BR-C patients were more likely to suffer major complications (30.8% vs. 25.9%, p<0.001) and mortality (4.1% vs. 2.3%, p<0.001). In addition, BR-C patients with major complications suffered a 50% higher mortality rate compared to non-BR-C patients with major complications (11.5% vs. 7.7%, p<0.001). For BR-C patients, multivariate analysis identified the following risk factors for major complications: albumin<3.5g/dL (odds ratio, OR-1.24, p=0.036), dyspnea (OR-1.71, p<0.001), preoperative sepsis (OR-1.89, p=0.001), age≥80 (OR-1.56, p<0.001), lack of independent function (OR-1.92, p<0.001), and intraoperative transfusion≥4 units (OR-2.14, p<0.001). Independent factors associated with mortality included: anesthesia risk score>3 (OR-2.27, p=0.025), age≥80 (OR-2.83, p<0.001), lack of independent function (OR-2.89, p=0.002), and intraoperative transfusion ≥4 units (OR-2.80, p=0.003).
Conclusions: These data confirm that a large number of medically high-risk patients are being treated with PD. These BR-C patients were at higher risk for and less able to be rescued from major morbidity, with higher rates of mortality from potentially reversible risk factors. These data suggest the need for optimization of comorbidities and for increased utilization of prehabilitation to address nutritional and conditioning deficits before PD.
Back to Annual Meeting Program
|