|
Back to Annual Meeting Program
Molecular Pathological Phenotypes and Outcome in Pancreatic Ductal Adenocarcinoma
Nigel B. Jamieson*1, Mohamed a. Mohamed1, Karin Oien2, Fraser Duthie2, Euan J. Dickson1, Ross Carter1, Colin Mckay1
1West of Scotland Pancreatic Unit, Glasgow University Department of Surgery, Glasgow Royal Infirmary, Glasgow, United Kingdom; 2Department of Pathology, Southern General Hospital, University of Glasgow, Glasgow, United Kingdom
Introduction: Individuals with pancreatic ductal adenocarcinoma (PDAC) demonstrate a generally poor outcome following resection. Molecular profiling has previously enhanced the identification of phenotypic subtypes of ampullary adenocarcinoma. Furthermore an intestinal subtype of PDAC has been described however the prognostic impact of this variant has not been described in detail. We sought to better characterize the intestinal subgroup of PDAC and assess the impact on outcome.
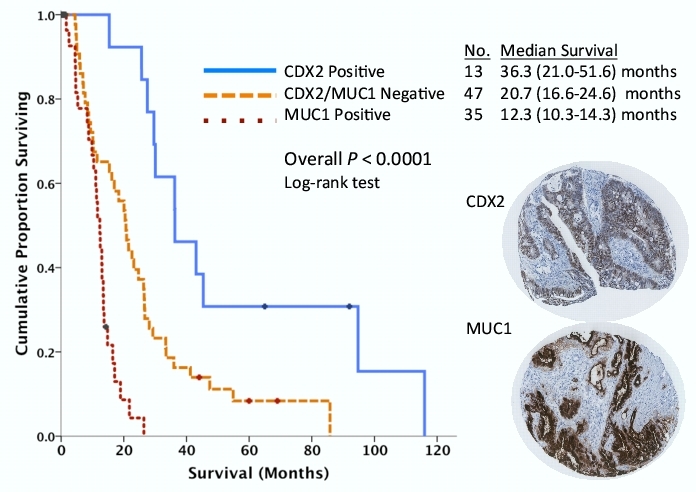
Methods: We assessed the potential clinical utility of molecular pathological phenotypes defined using a combination of histopathology and protein expression (CDX2 [caudal-type homeodomain transcription factor 2] - an intestinal marker and MUC1 - a pancreaticobiliary marker) assessed by immunohistochemistry (Figure 1) in 95 patients who underwent operative resection for PDAC by pancreaticoduodenectomy at a single institution over a 12 year time period. A tissue microarray was used with at least 4 cores evaluated for each tumor for protein expression analysis in addition to whole section analysis of tumor morphology. Care was taken to exclude all other periampullary malignancies from the analysis.
Results: In addition to prognostic impact of T stage, lymph node status, resection margin status, perineural invasion and vascular invasion, a small proportion of tumors had features of an intestinal histological subtype (13%) and a more favorable prognosis. CDX2 and MUC1 expression were significant prognostic variables. Patients with CDX2 negative tumors had a significantly shorter survival (Hazard ratio [HR] = 2.77, 95%CI: 1.5-5.2, P = 0.002 as did those with MUC1 positive tumors (HR = 2.89, 95%CI: 1.7-4.9, P < 0.0001 - no survivors at 24 months). Patients with CDX2 negative/MUC1 negative tumors had an intermediate outcome (Figure 1). In a multivariate analysis lymph node involvement, vascular invasion, positive MUC1 expression and loss of CDX2 expression were independent predictors of poor outcome.
Conclusion: Morphological determination of intestinal subtype of PDAC has clinical relevance. Furthermore maintenance of CDX2 expression identifies a group of PDAC patients with a relatively good outcome while MUC1 expression identified patients with a very poor outcome. When combined histopathological and molecular criteria define clinically relevant phenotypes of PDAC with significant implications for prognostication, current therapeutic strategies and may facilitate future trial design.
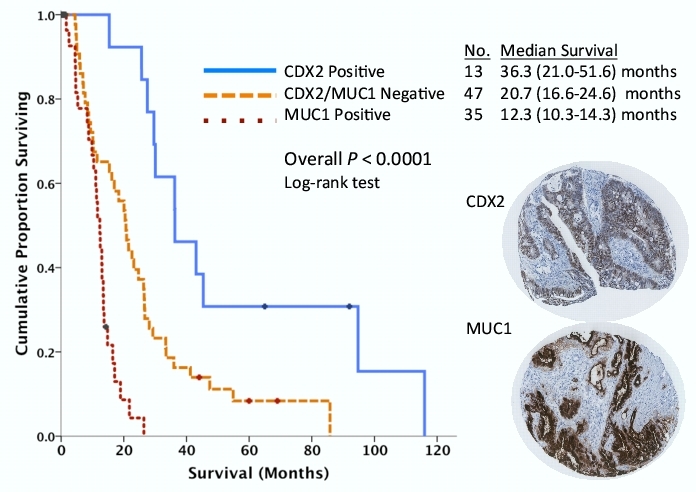
Figure 1. Kaplan-Meier survival curves demonstrating stratification of the 95 patient PDAC cohort according to CDX2 and MUC1 expression assessed by immunohistochemistry.
Back to Annual Meeting Program
|