|
 |
Back to Annual Meeting Program
Transplant Versus Resection for the Management of Hepatocellular Carcinoma in the Post-2006 MELD Exception Era At a Single Institution in the Southeast UNOS Region
Malcolm H. Squires*1, Steven Hanish2, Sarah B. Fisher1, Cristen Garrett2, David Kooby1, Juan M. Sarmiento3, Kenneth Cardona1, Stuart J. Knechtle2, Maria C. Russell1, Joseph F. Magliocca2, Andrew B. Adams2, Charles a. Staley1, Shishir K. Maithel1
1Department of Surgery, Division of Surgical Oncology, WInship Cancer Institute, Emory University, Atlanta, GA; 2Department of Surgery, Division of Liver Transplantation, Emory Transplant Center, Emory University, Atlanta, GA; 3Department of Surgery, Division of General and GI Surgery, Emory University, Atlanta, GA
Background: Optimal management of hepatocellular carcinoma (HCC) in the post-2006 MELD (Model for End Stage Liver Disease) exception era remains controversial and is regionally dependent. We compared outcomes for patients undergoing liver transplant versus resection at a single institution in a UNOS region with short wait times for organ availability.
Methods: All patients who underwent resection of HCC between 1/00 and 8/12 were identified. Inclusion of patients who underwent transplant was limited to those after 1/06, when the MELD exception policy for HCC based on the Milan criteria (MC) was universally incorporated into UNOS organ allocation. Primary outcomes were overall survival (OS) and recurrence-free survival (RFS).
Results: 259 patients were identified, of whom 133 underwent transplant and 126 underwent resection. Transplant patients had a higher incidence of hepatitis C (67% vs 29%, p<0.001), a greater median raw MELD score (15 vs 8, p<0.001), and smaller tumor size (2.4 vs 7.0 cm, p<0.001). All 133 patients who underwent transplant met MC, while 37 (29%) who underwent resection met MC. Of these 37 patients, 26 had preserved liver function with a raw MELD score ≤8. Median follow-up time was 30 mos. Median wait time to transplant was 55 days (1-321); no patients dropped off the waitlist while awaiting an organ.
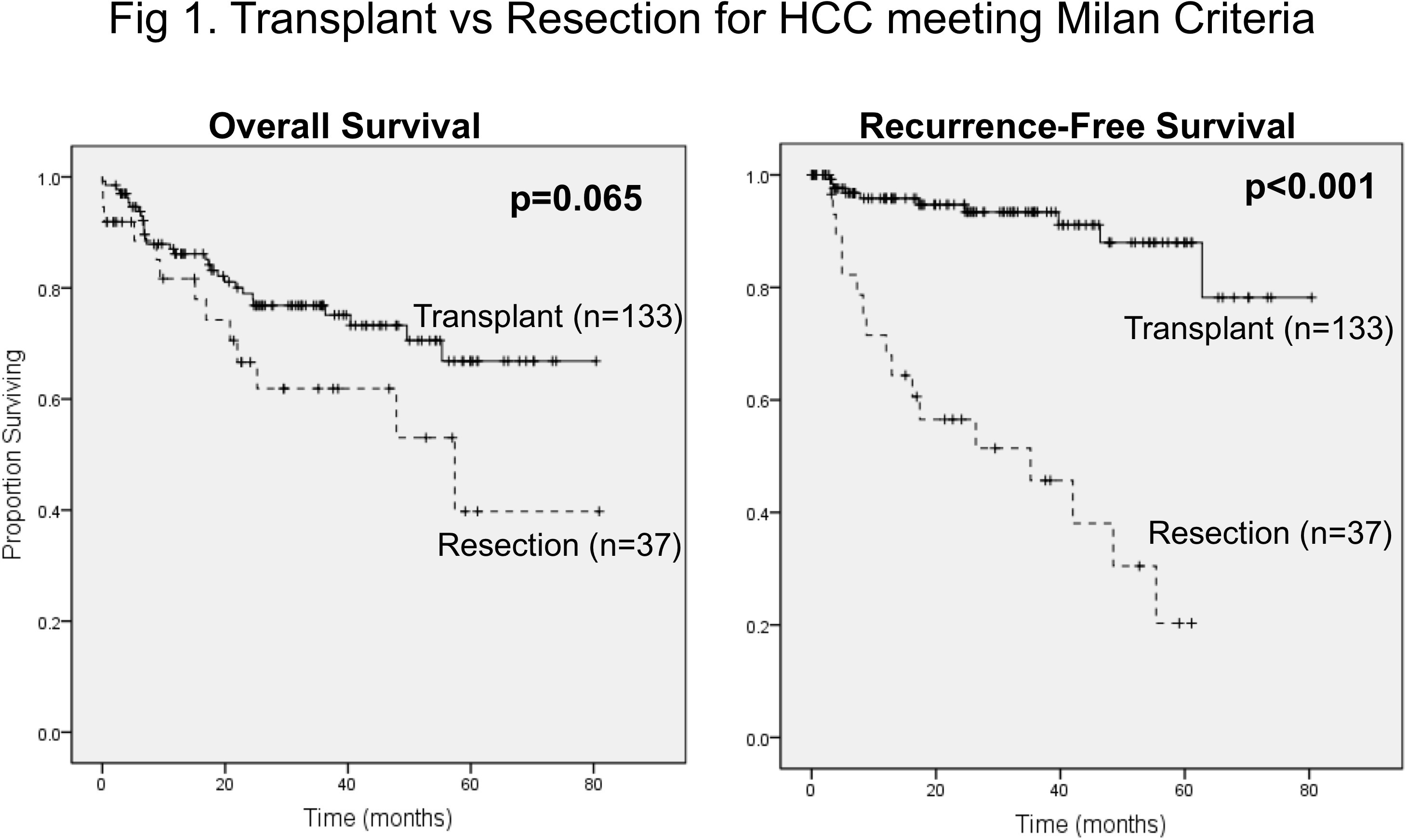
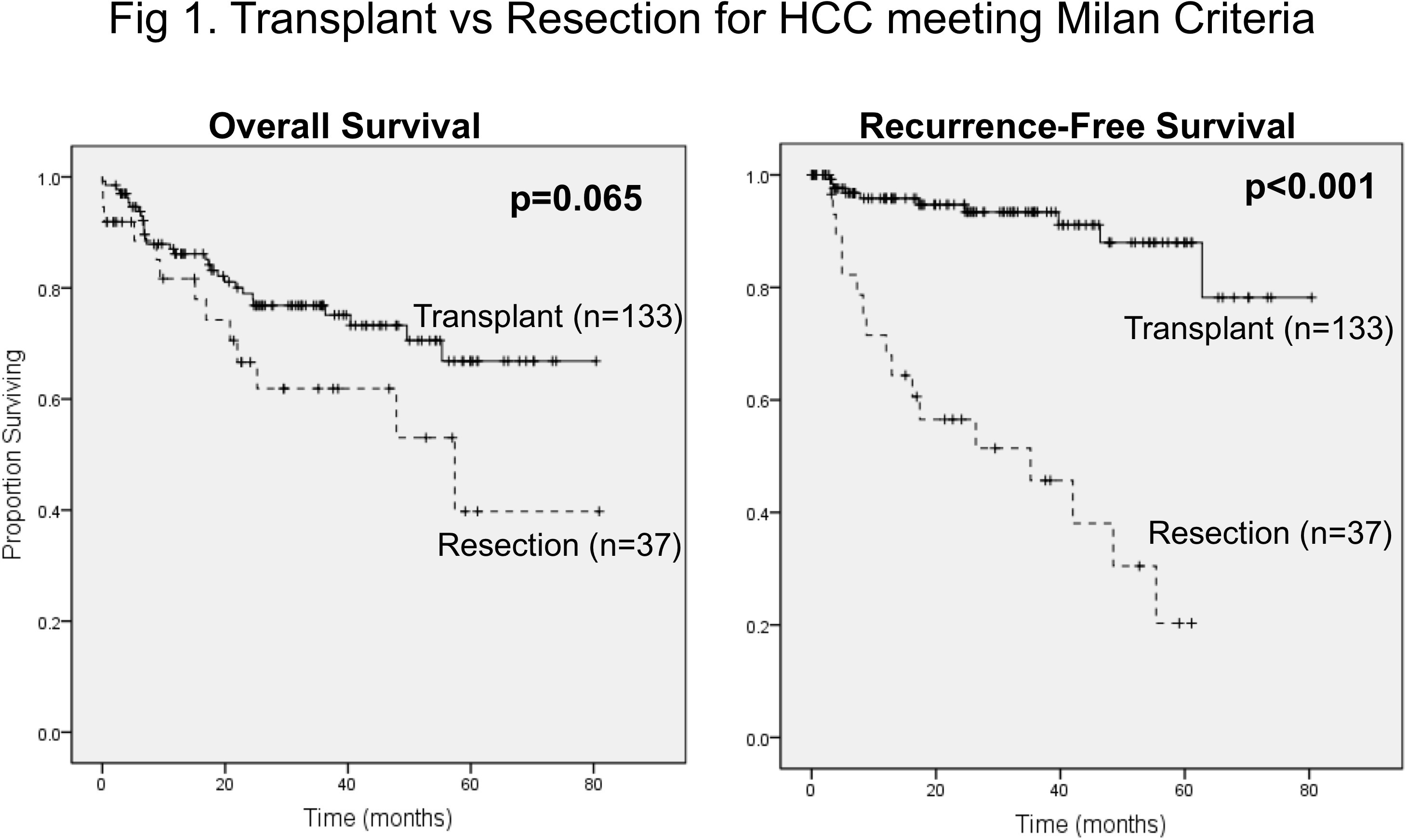
Transplant compared to resection was associated with improved OS (median not reached (MNR) vs 28.7 mos, p<0.001) and greater RFS (MNR vs 17.4 mos, p<0.001). When compared to the 37 patients within MC who underwent resection, transplant demonstrated a trend towards improved OS (MNR vs 57.4 mos, p=0.065) and greater RFS (MNR vs 35.2 mos, p<0.001; Fig). Of these 37 patients who underwent resection, 11 (30%) have undergone salvage procedures for recurrence of HCC versus only 4 (3%) transplant patients. Compared to resection patients within MC with a raw MELD score ≤8 (n=26), transplant demonstrated similar OS (MNR vs 57.4 mos, p=0.84) but greater RFS (MNR vs 17.6 mos, p<0.001). For patients with hepatitis C, those undergoing transplant (n=89) had improved outcomes compared to the 19 patients who met MC and underwent resection (OS: MNR vs 47.9 mos, p=0.04; RFS: MNR vs 16.2 mos, p<0.001).
Conclusion: In a region with short wait times for organ availability, liver transplant is associated with improved survival compared to resection for HCC. For patients within Milan criteria, transplant appears to confer an oncologic advantage as well, even in those with preserved liver function. For patients within Milan criteria with hepatitis C, transplant is associated with improved survival and decreased recurrence when compared to resection. Transplant should be considered for all patients meeting Milan criteria, particularly those with hepatitis C, when being managed in a region with short wait times for organ availability.
Back to Annual Meeting Program
|