|
 |
Back to Annual Meeting Program
Limitations of NSQIP in Reporting Complications for Patients Undergoing Pancreactectomy: Underscoring the Need for a Pancreas-Specific Module
Irene Epelboym*, Irmina Gawlas, James a. Lee, Beth Schrope, John a. Chabot, John D. Allendorf
Surgery, Columbia University Medical Center, New York, NY
Background:
Administrative databases are used with increased frequency for reporting hospital-specific and nationwide trends and outcomes after various surgical procedures in order to improve quality of surgical care. NSQIP is a risk-adjusted case-weighted complication tracking initiative that reports 30-day outcomes from more than 400 academic and community institutions in the United States alone. However, the accuracy of reported events specific to pancreatic surgery has never been reported in depth.
Methods:
We retrospectively reviewed a randomly selected subset of patients, the information on whose postoperative course was originally reported through NSQIP. Preoperative characteristics, operative data, and postoperative events were recorded after review of electronic medical records including physician and nursing notes, operative room records and anesthesiologist reports. We compared categorical variables using chi-square or Fischer's exact test and continuous variables using Student's t-test.
Results:
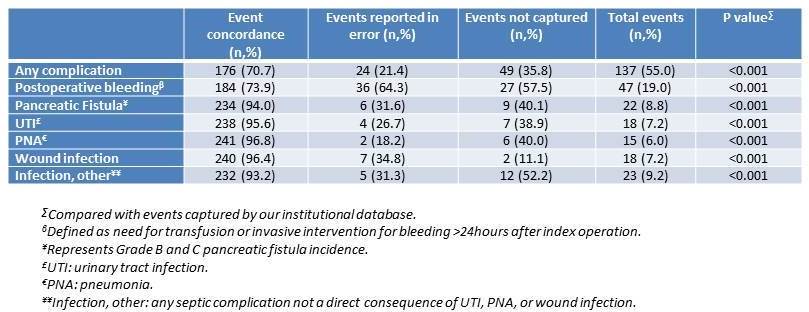
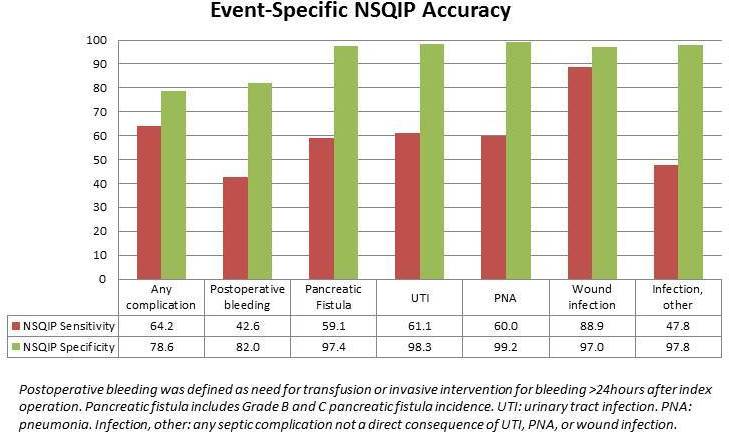
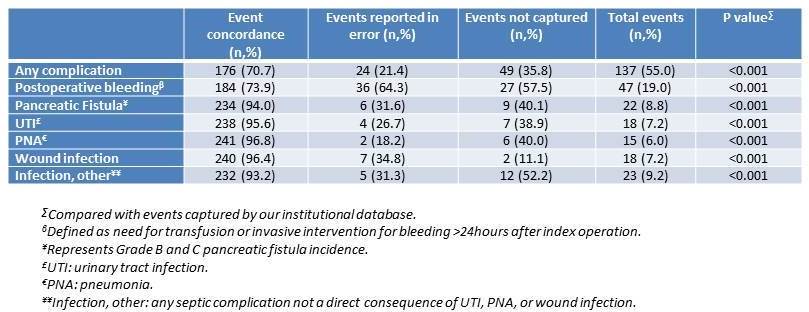
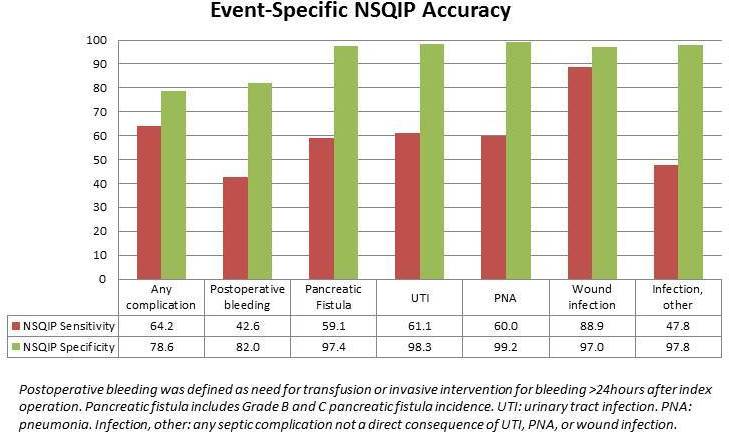
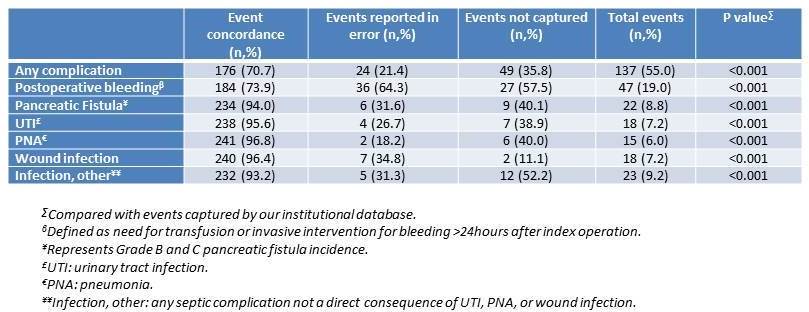
Between 2006 and 2010, 316 pancreatectomy cases were reported to NSQIP by our institution. Two hundred and forty-nine were reviewed in detail, among them 145 (58.2%) Whipples, 19 (7.6%) total pancreatectomies, 65 (26.1%) distal pancreatectomies, and 15 (6.0%) central or partial resections. Median age was 65.7, males comprised 41.5% of the group, and 74.3% of patients were Caucasian. Overall rate of complications reported by NSQIP was 44.0%, compared with 55.0% in our review, however discordance was observed in 73 (29.3%) cases (p<0.001), including 24 cases of reporting a complication where there was not one, and 49 cases of missed complication. Most frequently reported event was postoperative bleeding requiring transfusion (22.7%), however true incidence of postoperative bleeding was actually 19.0%, with NSQIP missing 27 (57.5%) and incorrectly reporting 36 (64.3%), p<0.001. Four procedures unrelated to the index operation were recorded as reoperation events. While a pancreas-specific module does not yet exist, NSQIP reports a 7.6% rate of organ-space surgical site infections; when compared with our institutional rate of Grade B and C postoperative fistula (8.8%), we observed discordance 6% of the time, p<0.001. Delayed gastric emptying, a common post-pancreatectomy morbidity, was not captured at all. Additionally, there were significant inaccuracies in reporting urinary tract infections, postoperative pneumonia, wound complications, and postoperative sepsis, with discordance rates of 4.4%, 3.2%, 3.6%, and 6.8%, respectively.
Conclusions:
NSQIP data is an important and valuable tool for evaluating quality of surgical care, however pancreatectomy-specific postoperative events are often misclassified, underscoring the need for a hepatopancreatobiliary-specific module to better capture key outcomes in this complex and unique patient population.
Back to Annual Meeting Program
|