|
|
Back to Annual Meeting Program Tumor Size Does Not Dictate Prognosis After Resection for Hepatocellular Carcinoma. Results From a Large Western Series Michael D. Kluger*1,2, Andrea Belli2, Alexis Laurent2, Daniel Azoulay2, Daniel Cherqui1,2 1Division of Hepatobiliary Surgery and Liver Transplantation, New York-Presbyterian Hospital Weill Cornell Medical College, New York, NY; 2Service de Chirurgie Digestive et Hépatobiliaire, Hôpital Henri Mondor, Assistance Publique-Hôpitaux de Paris -Université Paris-Est, Créteil, France
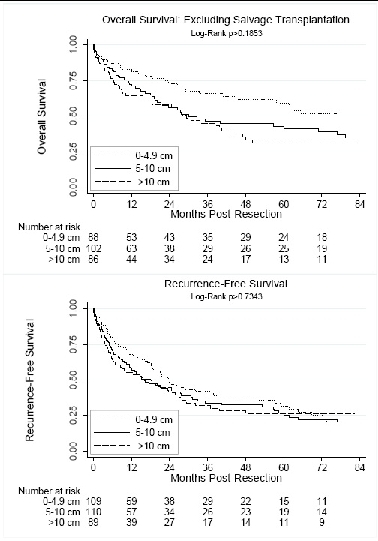
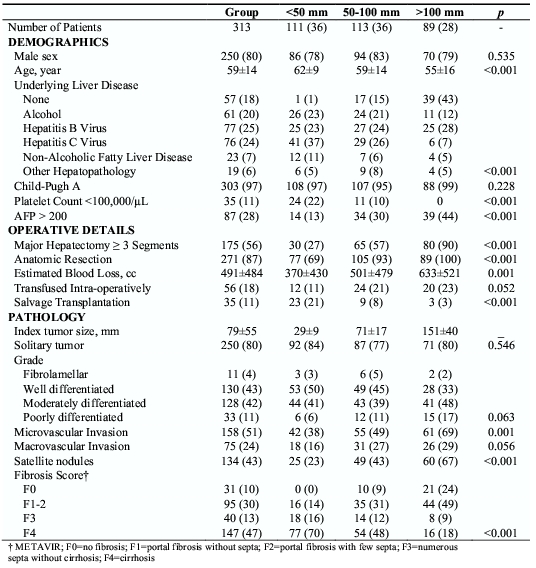
INTRODUCTION: Operative management remains the gold standard approach for hepatocellular carcinoma (HCC). Resection is the preferred treatment in patients without cirrhosis, with transplantation being the best option for decompensated cirrhotics. This study evaluated underlying liver disease, operative factors and histopathological characteristics on overall and recurrence-free survival in 313 patients undergoing liver resection for HCC at a single Western center. METHODS: Patients who underwent liver resection for HCC between 3/89 and 9/10 were studied. Patients were not excluded based on tumor size, extent of fibrosis, or etiology of underlying liver disease. As indications for treatment are mostly based on tumor size, patients were stratified by diameter: < 50 mm, 50-100 mm and > 100 mm. Patients with Child's A cirrhosis, no esophageal varices, and a platelet count ≥100 × 10^9/L were directed toward resection. Kaplan-Meier and Cox regression methodology were utilized. RESULTS: 36% had tumors <50 mm, 36% had tumors 50-100 mm, and 28% had tumors > 100 mm. Patients with larger tumors were more likely to have normal underlying liver parenchyma: 43% > 100 mm, 15% 50-100 mm and 1% < 50 mm (p <0.001). 77% underwent an open and 23% a laparoscopic procedure (p<0.001). Major hepatectomies comprised 56%, anatomic resections 87%, and R0 88% of resections. There was no significant difference in Clavien 3-5 complications among the groups (p=0.78), 16% overall. This rate decreased in the second decade of our experience. For example, the mortality rate between 3/89 and 12/99 was 14%, and 5% through 9/10 (p<0.008). Median overall survival was 60 months, with 1- and 5-year overall survival rates of 76% and 50%. On multivariate analyses, intra-operative transfusion (HR=2.60), cirrhosis (HR=2.42), salvage transplantation (HR=0.23), poorly differentiated tumor (HR=2.04), satellite lesions (HR=1.68), microvascular invasion (HR=1.48), and AFP > 200 (HR=1.53) were significant predictors of survival. Median time to recurrence was 20-months, with 1- and 5-year recurrence-free survival rates of 61% and 28%. By multivariate analyses intra-operative transfusion (HR=2.15), poorly differentiated tumor (HR=1.87), cirrhosis (HR=1.69) and microvascular invasion (HR=1.71) independently impacted recurrence-free survival. CONCLUSION: It is demonstrated that resection is a safe and readily available treatment for any size HCC in properly selected patients in the modern era of liver surgery. Tumor size did not independently impact recurrence or survival on multivariate analyses, whereas tumor histopathology and background parenchyma did. The current investigation adds to a growing body of literature supporting that HCC tumor biology and the condition of the non-tumor parenchyma should be given greater consideration in considering resection in this era of organ shortage. Back to Annual Meeting Program
|
|||||||
© 2026 Society for Surgery of the Alimentary Tract. All Rights Reserved. Read the Privacy Policy.