|
 |
Back to Annual Meeting Program
Simultaneous Surgical Resection of Primary and Metastatic Carcinoid and Neuroendocrine Tumors Is Both Safe and Effective
Nicholas N. Nissen*1, Vijay G. Menon1, Edward M. Wolin2, Run Yu2, James M. Mirocha3, Alagappan Annamalai1, Deepti Dhall4, Ashley Wachsman5, Marc L. Friedman5, Steven D. Colquhoun1
1Hepatobiliary and Pancreatic Surgery, Cedars-Sinai Medical Center, Los Angeles, CA; 2Carcinoid and Neuroendocrine Tumor Program, Cedars-Sinai Medical Center, Los Angeles, CA; 3Biostatistics, Cedars-Sinai Medical Center, Los Angeles, CA; 4Pathology, Cedars-Sinai Medical Center, Los Angeles, CA; 5Radiology, Cedars-Sinai Medical Center, Los Angeles, CA
Introduction: Management strategies for patients with carcinoid and neuroendocrine tumors (CNETs) generally include removal of the primary tumor and cytoreduction (CR) of metastatic tumor burden, both to improve survival and control symptoms. Patients with synchronous presentation of primary tumors and hepatic metastases present a unique challenge. We reviewed our experience with simultaneous surgical removal of primary abdominal CNETs and hepatic metastases.
Patients: Forty-seven patients underwent simultaneous hepatic resection and removal of either small bowel carcinoid (n=32) or pancreatic NET (n=15) by two experienced hepatobiliary surgeons as part of a multidisciplinary CNET treatment group. Surgical details are shown in the Table. In 22 patients, surgery was undertaken with a goal of near total surgical CR, while in 25 patients partial surgical CR was performed as part of a plan to include postoperative hepatic arterial or ablative therapy. Tumor progression was categorized using RECIST criteria.
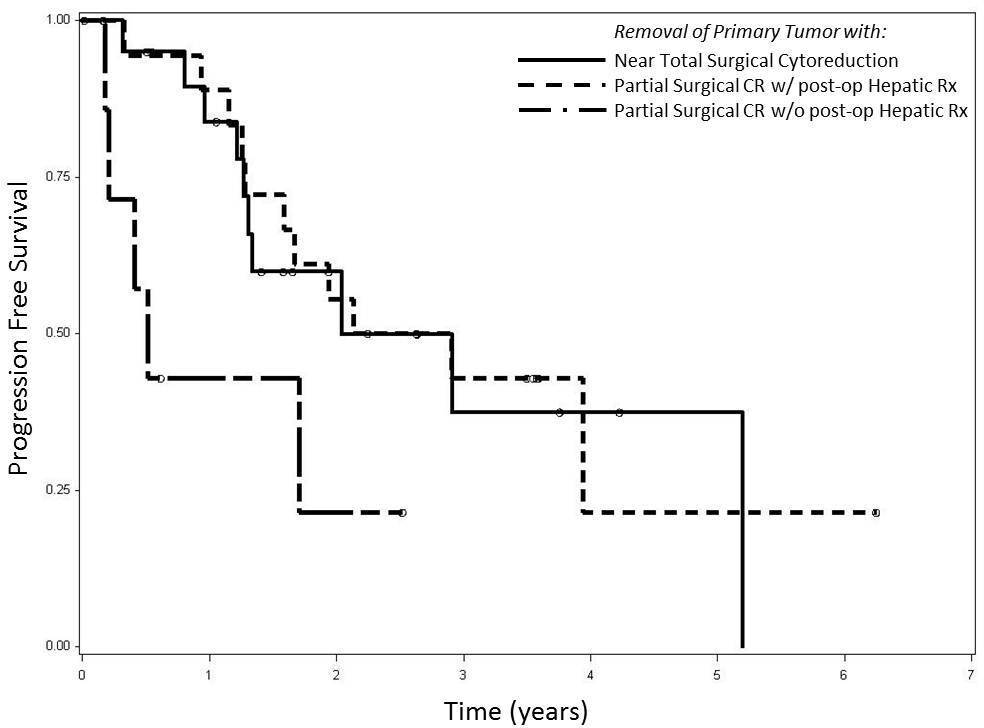
Results: Nineteen patients had carcinoid syndrome and all had dramatic improvement after surgery, with complete resolution in 11 (58%) cases. Overall there were 8 complications of Clavien grade > 2 including bile leak requiring ERCP (n=2) and repeat laparotomy (n=4). There was no 30-day mortality. Median length of stay was 7 days. Overall survival for the entire cohort at 1, 3 and 5 years was 95%, 82% and 82%, while the progression free survival at 1, 3 and 5 years was 77%, 37% and 28%. In the 22 patients undergoing near total surgical CR, no patient required repeat hepatic intervention within 12 months. In the 25 patients undergoing partial surgical CR, 18 (72 %) went on to receive postoperative hepatic treatments within 12 months. Progression free survival was similar in patients whether they underwent total CR or partial CR with staged hepatic treatment. Patients who failed to undergo postoperative hepatic therapy (n=7) were at increased risk of progression compared either to patients with near total CR (HR = 3.10, P = 0.044) or partial CR and staged liver treatment (HR = 3.37, P = 0.029) (Figure).
Conclusion: To our knowledge this series represents the largest single center report of simultaneous resection of primary abdominal CNETs and hepatic metastases in the literature. Our results demonstrate that this surgical approach is safe and effective in expert hands. In patients undergoing near total hepatic CR, which made up almost half of our series, no additional hepatic treatments were required over the next year, which in turn demonstrates the effective consolidation of treatments into a single surgical endeavor. In remaining patients, resection of the primary tumor combined with partial hepatic CR combined with postoperative hepatic therapy was equally effective. A multidisciplinary and multimodal approach is essential in these patients.
Variables Associated with Simultaneous Resection
| Type of Primary Surgery | | | Small Bowel Resection | 21 | | Right Hemicolectomy | 12 | | Segmental or Distal Pancreatic Resection | 11 | | Pancreaticoduodenectomy | 3 | | Type of Liver Surgery | | | Major Resection of 3 or more segments | 9 | | Segmental Resection (1 or 2) | 11 | | Multiple Wedge Resections and Enucleations | 27 | | Largest Liver Tumor size (cm) | 4.9 (mean); 3.5 (median); 0.6-17 (range) | | No. of liver lesions resected; | 5.5 (mean); 3 (median); 1-28 (range) | | Grade; High : Intermediate : Low : N/s | 4.3% : 27.7% : 51.1% : 17% | | Differentiation; Poor : Well : N/s | 4.3% : 82.9% : 12.8% | | Positive Lymph nodes (%) | 78.6% | | R0 Resection (%) | 57.4% | | Bilobar Resection (%) | 55.3% | |
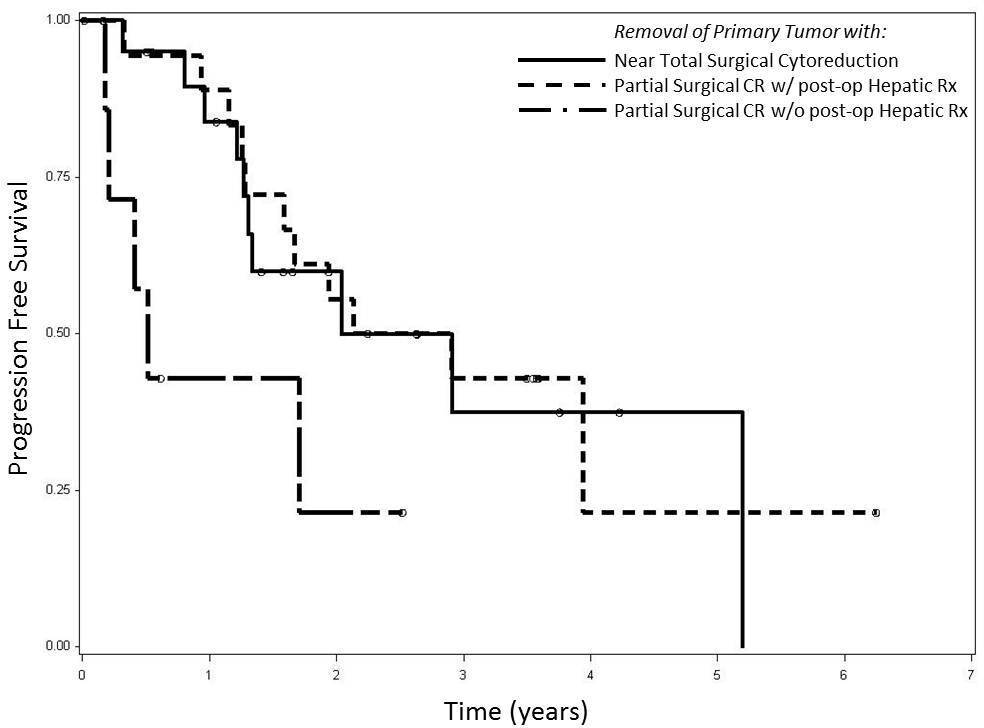
Progression Free Survival Related to Type of Cytoreductive Treatment
Back to Annual Meeting Program
|