|
|
Back to Annual Meeting Program Short-Term but Not Long-Term Patency of Venous Reconstruction During Pancreatic Resection Predicts Survival Irmina Gawlas*, Irene Epelboym, Megan Winner, Joseph Dinorcia, Yanghee Woo, James a. Lee, Beth Schrope, John a. Chabot, John D. Allendorf Department of Surgery, Columbia University, New York, NY
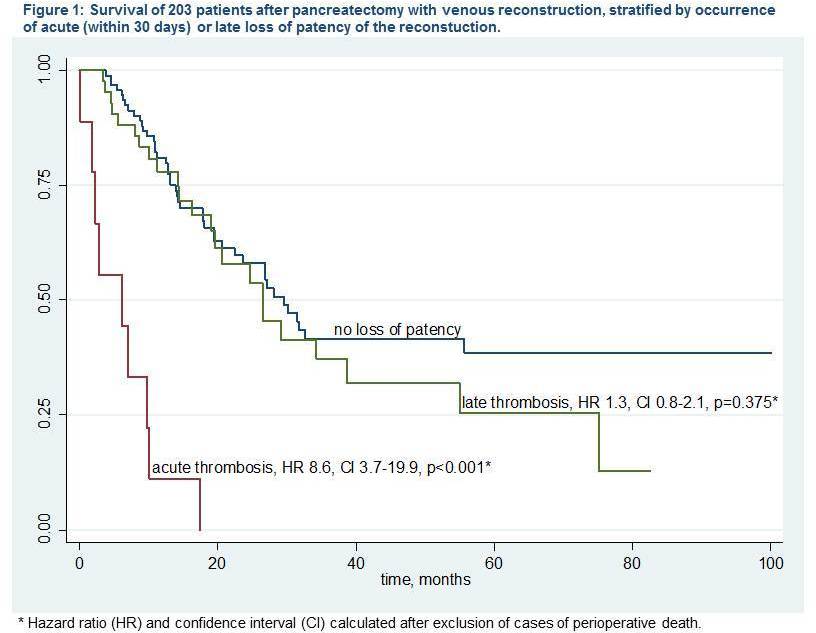
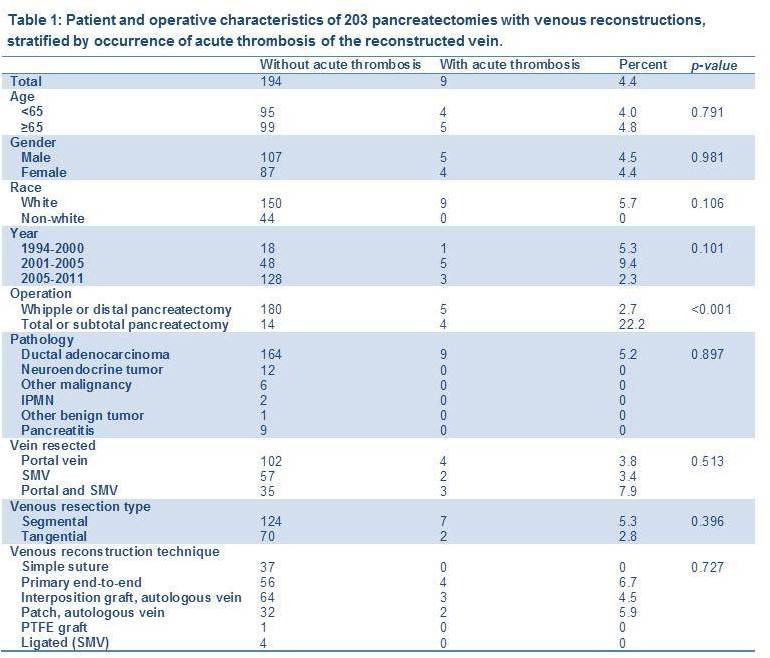
BACKGROUND Pancreatic surgery with concomitant vascular reconstruction is being performed with increasing frequency, and offers the benefits of surgical resection to patients with locally advanced disease. The technique is not standardized, however, and the short and long-term patency rates and the clinical significance of thrombosis of a reconstructed venous system are unknown. METHODS We reviewed clinical and operative characteristics as well as follow up records of patients who underwent pancreatic resections requiring venous resection and reconstruction from 1994 to 2011. We sought to identify predictors of acute (occurring within 30 days) thrombosis of the venous reconstructions using logistic regression, and predictors of late loss of patency using Cox-proportional hazards. We compared survival of patients with thrombosis of the mesenteric venous system to that of patients with patent reconstructions. RESULTS Between 1994 and 2011, 203 pancreatic operations requiring venous reconstruction were performed. Of these, 106 (52.2%) included resection of the portal vein (PV), 59 (29.1%) included the superior mesenteric vein (SMV) only, and in 38 (18.7%) patients, the confluence of the PV and SMV was resected. Segmental resection was performed in 131 (64.5%), and 72 (35.5%) underwent tangential resection. Ninety-seven veins (47.8%) were repaired primarily, 67 (33.0%) were repaired using a venous interposition graft, and 34 (16.8%) were repaired using an autologous vein patch. Acute thrombosis occurred in 9 (4.4%) cases, and was significantly associated with increased perioperative mortality (22.2% versus 4.6%, p=0.023). After excluding cases of perioperative mortality, acute thrombosis was associated with decreased median survival (7.1 versus 15.9 months, p=0.011) and increased hazard of death (HR 8.6, CI 3.7-19.9, p<0.001). These events were more common in cases of total or subtotal resection compared to Whipple or distal resections (22.2 versus 2.7%, p<0.001). Long-term follow-up imaging was available for 138 patients at a median of 11.7 months. Of these, 43 (31.2%) experienced a loss of patency of the portal venous system at a median of 9.5 months; the majority of these were associated with tumor recurrence. Independent predictors of late loss of patency were age under 65 (HR 2.2, CI 1.2-4.1, p=0.015) and segmental resection (HR 3.3, CI 1.5-7.2, p=0.002). Later loss of patency was not associated with decreased median survival (18.1 versus 16.8 months, p=0.455) or increased hazard of death (HR 1.3, CI 0.8-2.1, p=0.375). CONCLUSIONS Acute thrombosis of the reconstructed portal venous system after pancreatic surgery is clinically significant; it is associated with increased perioperative mortality, and even when non-fatal, is associated with decreased survival. Late loss of patency occurs in one-third of patients but does not affect survival. Back to Annual Meeting Program
|
|||||||
© 2026 Society for Surgery of the Alimentary Tract. All Rights Reserved. Read the Privacy Policy.