|
Back to Annual Meeting Program
Night Time Is Not the Right Time: Increased Risk of Complications After Laparoscopic Cholecystectomy At Night
Uma R. Phatak*, Curtis J. Wray, Debbie Lew, Richard Escamilla, Winston M. Chan, Tien C. Ko, Lillian S. Kao
Surgery, University of Texas Health Science Center, Houston, TX
Evidence from a large national database has shown that performance of non-emergent general surgery procedures at night does not predispose patients to increased morbidity or mortality. However, these results may not be generalizable to high risk populations of medically underserved patients. We hypothesized that performance of laparoscopic cholecystectomy (LC) at night in such a population would be associated with increased post-operative complications.
We conducted an IRB approved single center retrospective review of consecutive LC patients between October 2010 and May 2011 at a safety-net hospital in Houston, TX. Data were collected regarding demographics, date and site of diagnosis (defined as first imaging study demonstrating gallstones), number of biliary-related admissions and emergency room (ER) visits between diagnosis and surgery, length of stay (LOS) for each admission, dates and types of procedures, dates and types of imaging studies, and 30-day postoperative complications (bile leak/biloma, common bile duct injury, retained stone, superficial surgical site infection, organ space abscess, pneumonia, readmission, and death). We defined "night" as 7PM to 7AM. Statistical analyses were done using STATA 12 (College Station, TX).
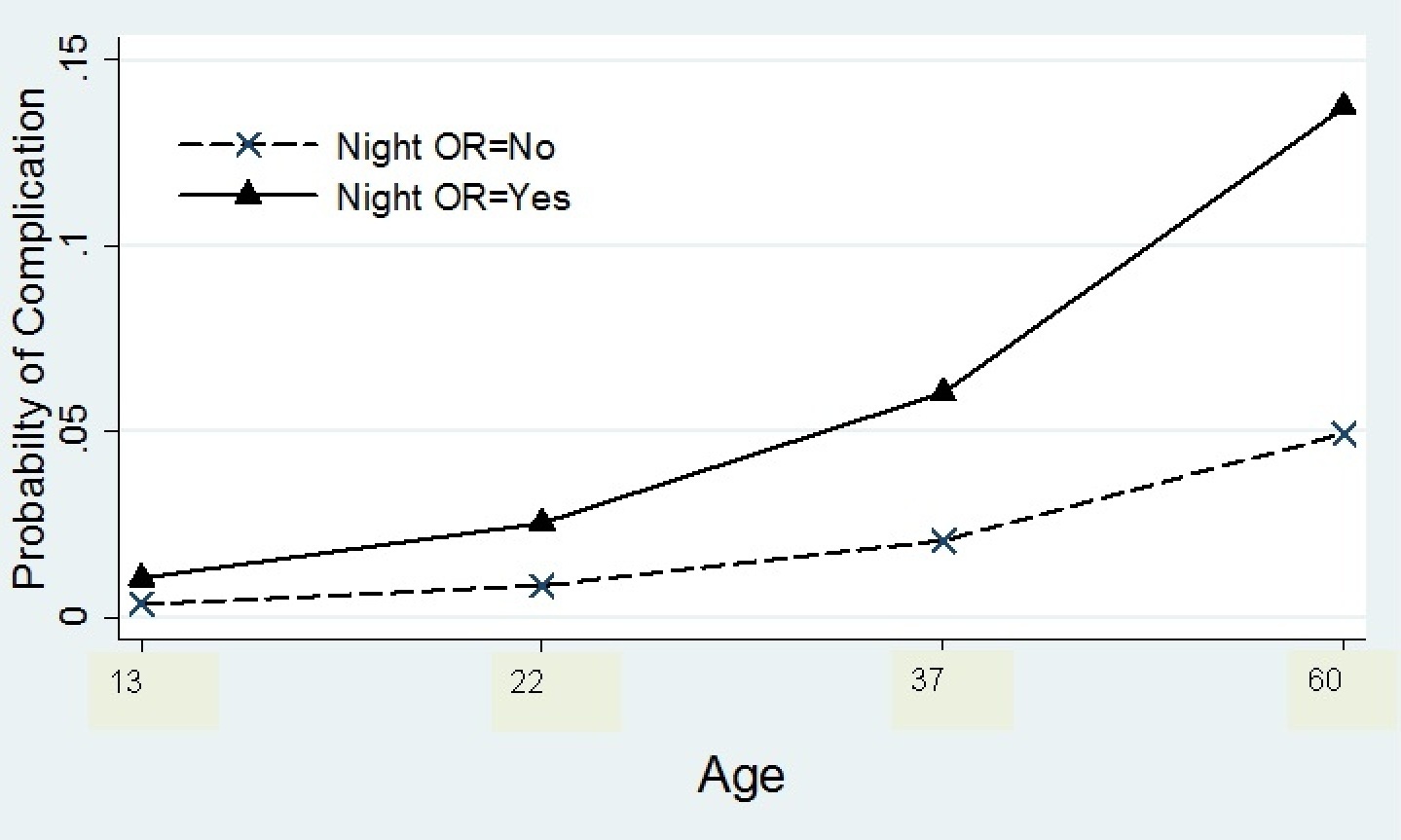
During the 8-month period, 580 patients received LC and incision times were available for 549. Of these 38% (n=208) were elective and 62% (n=341) were non-elective. A majority were female (n=460, 84%) and Latino (n=456, 83%). There were 196 LC performed at night of which 186 were non-elective and 10 were elective. Of the 353 daytime LCs, 198 were elective and 155 were non-elective. There were 35 complications in 22 patients (4 elective, 18 non-elective). Multivariate analysis revealed age (OR 1.05, 95% CI 1.01 to 1.08, p=0.003) and LC at night (OR 3.1, 95% CI 1.3 to 7.6, p=0.012) to be associated with increased risk of complications. The predicted probability of a complication increased three fold for older patients who received LC at night (Figure).
Age and performance of LC at night were predictive of an increased risk of complications among medically underserved patients treated at a high volume safety net hospital with limited resources. Restricting performance of LCs to the daytime in high risk patients, such as the elderly, may lead to improved outcomes in this challenging clinical setting.
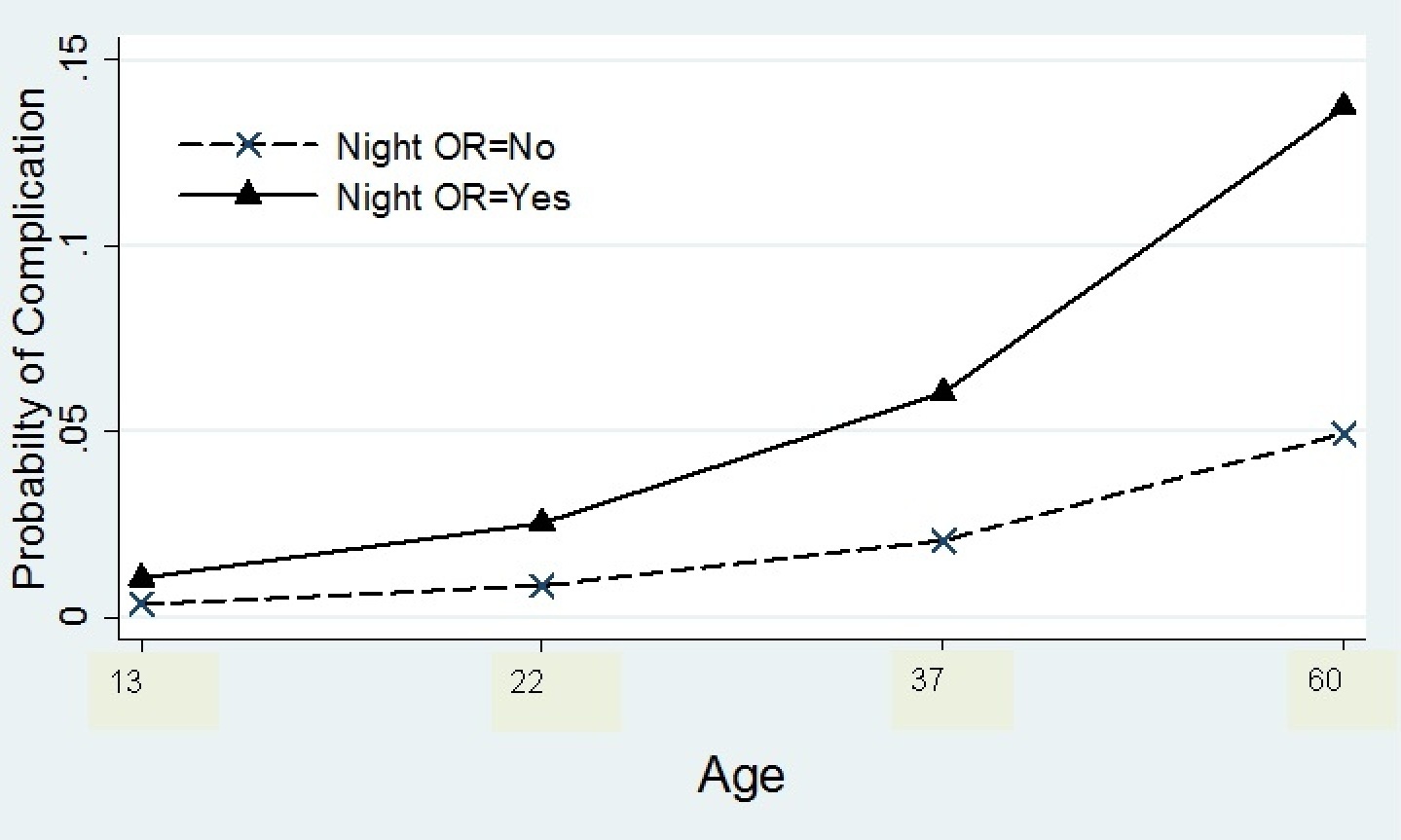
Predicted probability of complication after LC at night by age
Back to Annual Meeting Program
|