|
 |
Back to Annual Meeting Program
Extended Duration Thromboprophylaxis Cost-Effectiveness in Abdominal Surgery
James C. Iannuzzi*1, Aaron S. Rickles1, James G. Dolan2, Fergal Fleming1, John R. Monson1, Katia Noyes1
1Surgical Health Outcomes & Research Enterprise, Division of Colorectal Surgery, Department of Surgery, University of Rochester Medical Center, Rochester, NY; 2Community and Preventative Health, University of Rochester Medical Center, Rochester, NY
Background:
Post-discharge thromboprophylaxis is the practice of prescribing antithrombotic therapy for 21 days after discharge, commonly used in surgical patients who are at high risk for venothromboembolism (VTE). Multiple consensus guidelines recommend extended duration thromboprophylaxis (EDTPPX) after major abdominal oncologic resections based on randomized clinical trials demonstrating a significant reduction in VTE events after surgical discharge in these patients. While the National Comprehensive Cancer Network suggests all major abdominal oncologic resections receive EDTPPX, the American College of Chest Physicians suggests an individualized risk assessment, with only high risk patients undergoing oncologic resections suggested to receive EDTPPX, however, high risk is not currently defined. The threshold for high risk ought to be informed by when it is cost-effective to provide EDTPPX, which has not previously been established. In order to further inform current guidelines this study sought to determine the VTE incidence threshold for the cost-effectiveness of low molecular weight heparin for 4 weeks after surgery as compared to inpatient prophylaxis only.
Methods:
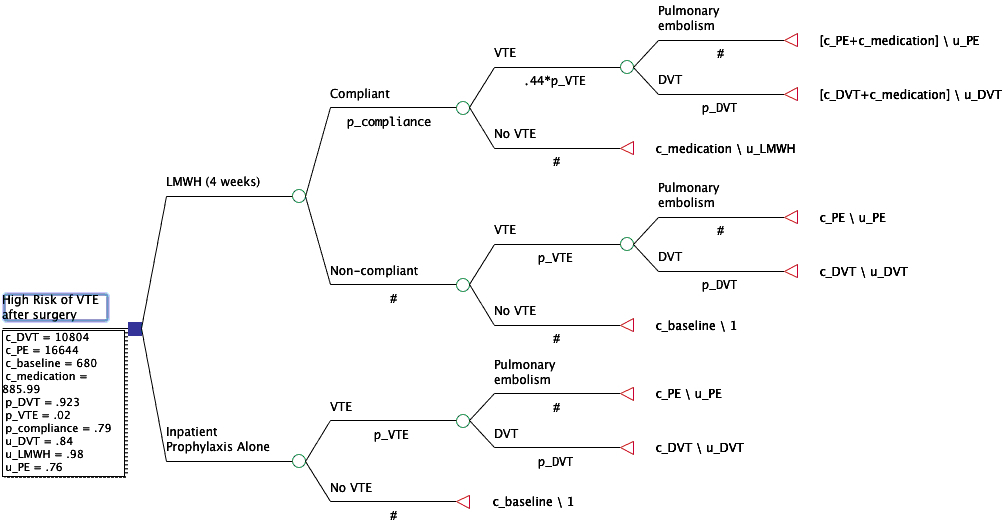
A cost-effectiveness decision tree was created using TreeAge (Figure 1). Assigned probabilities were derived from published literature. The decision point compared extended duration thromboprophylaxis with low molecular weight heparin for 21 days after discharge to inpatient-prophylaxis alone, with base case assumptions (table 1) based on an abdominal oncologic resection without complications in a 45 year-old male. The end points were pulmonary embolism or deep vein thrombosis with attendant costs and assigned effectiveness evaluated by Quality Adjusted Life Years (QALY). Willingness to pay was set at $50,000/QALY. Sensitivity analyses were performed to assess uncertainty within the model, with particular interest in the threshold for cost-effectiveness based on VTE incidence.
Results:
Given base case assumptions with VTE probability of 4%, extended duration thromboprophylaxis had an incremental cost effectiveness ratio of $8123/QALY, which was considered cost-effective. The results were robust to sensitivity analysis with the highest uncertainty associated with VTE incidence and medication cost. The threshold for the relative cost-effectiveness was a VTE incidence exceeding 2.53%.
Conclusions:
Given the base case assumptions, extended prophylaxis is more cost effective than inpatient prophylaxis alone, and the threshold for its use should be cases where the estimated VTE risk exceeds 2.53%. These findings should inform future guidelines' definition of "high risk" and individualized risk scores should be developed to predict patient likelihood of post-discharge VTE. These results can lead to specific individualized EDTPPX application.
Table 1: Baseline Model Assumptions and Sensitivity Analysis
| Variable | Baseline Probability | Sensitivity Range | Cost ($,2010) | Cost Range ($) | Utility (range) | | VTE | 0.04 | 0.001-0.3 | N/A | N/A | N/A | | DVT | 0.923 | 0-.0923 | 10,804 | 3371-22,748 | 0.84 (0.7-0.931) | | PE | 0.077 | 0.077-1 | 16,644 | 6443-25,554 | 0.76 (0.6-0.89) | | LMWH | 0.22 | 0.22-0.7 | 885.99 | 357-885.99 | 0.98 (0.9-.099) | | No VTE | 0.96 | 0.7-0.999 | 680 | 0-680 | 1 |
VTE= Venothromboembolism, DVT=Deep Vein Thrombosis, PE= Pulmonary Embolism, LMWH= Low Molecular Weight Heparin
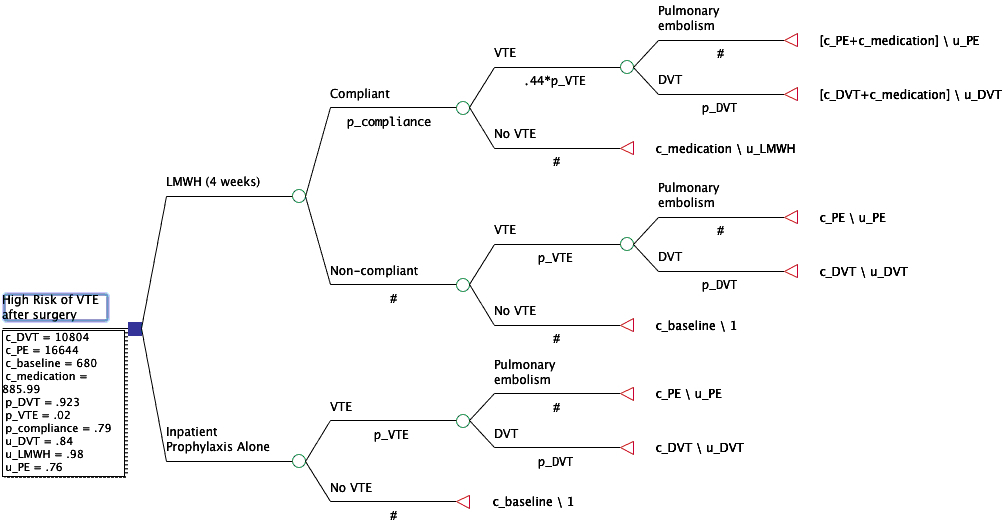
Figure 1: Decision Tree
Back to Annual Meeting Program
|