|
Back to Annual Meeting Program
Treatment Sequencing for Resectable Pancreatic Cancer: Influence of Early Metastases and Surgical Complications on Multimodality Therapy Completion Rates and Survival
Ching-Wei D. Tzeng*1, Daniel E. Abbott2, Jeffrey E. Lee1, Peter W. Pisters1, Jason B. Fleming1, Jean-Nicolas Vauthey1, Matthew Katz1
1Dept. of Surgical Oncology, The Univ. of Texas MD Anderson Cancer Center, Houston, TX; 2Surgical Oncology, University of Cincinnati, Cincinnati, OH
Introduction: Multimodality therapy (MMT) is important to the long-term survival of patients with resectable pancreatic adenocarcinoma (PDAC), but its completion can be hindered by early cancer progression or by treatment complications. We sought to compare the influence of each of these factors on the MMT completion rates of operable patients with resectable PDAC treated with either a neoadjuvant (NT) or surgery-first (SF) sequencing strategy.
Methods: We retrospectively evaluated all patients with PDAC at our institution from 2002-2007, who had 1) a radiographically resectable pancreatic head tumor, 2) a performance status (PS) and comorbidities suitable for immediate surgery, and 3) a carbohydrate antigen (CA) 19-9 <1000 U/ml. MMT was defined as resection before or after completion of planned pre- or post-operative therapy. Postoperative major complications (PMC) were defined as Clavien Grade ≥3. Disease progression was considered early when it developed within 3 months in SF patients or prior to planned resection in NT patients. Reasons for and rates of failure to complete MMT, 90-day PMC, and overall survival (OS) were compared between the two cohorts.
Results: 112 NT and 58 SF patients met inclusion criteria. 92/112 (82%) NT and 33/56 (59%) SF patients with complete follow-up completed MMT (p<0.001). NT patients did not complete MMT due to early progression (n=13, including 8 nontherapeutic laparotomies) and PS (n=7). SF patients did not complete MMT due to early progression (n=10), PMC (n=6), and PS (n= 3); 4 SF patients also underwent nontherapeutic laparotomy due to metastases.
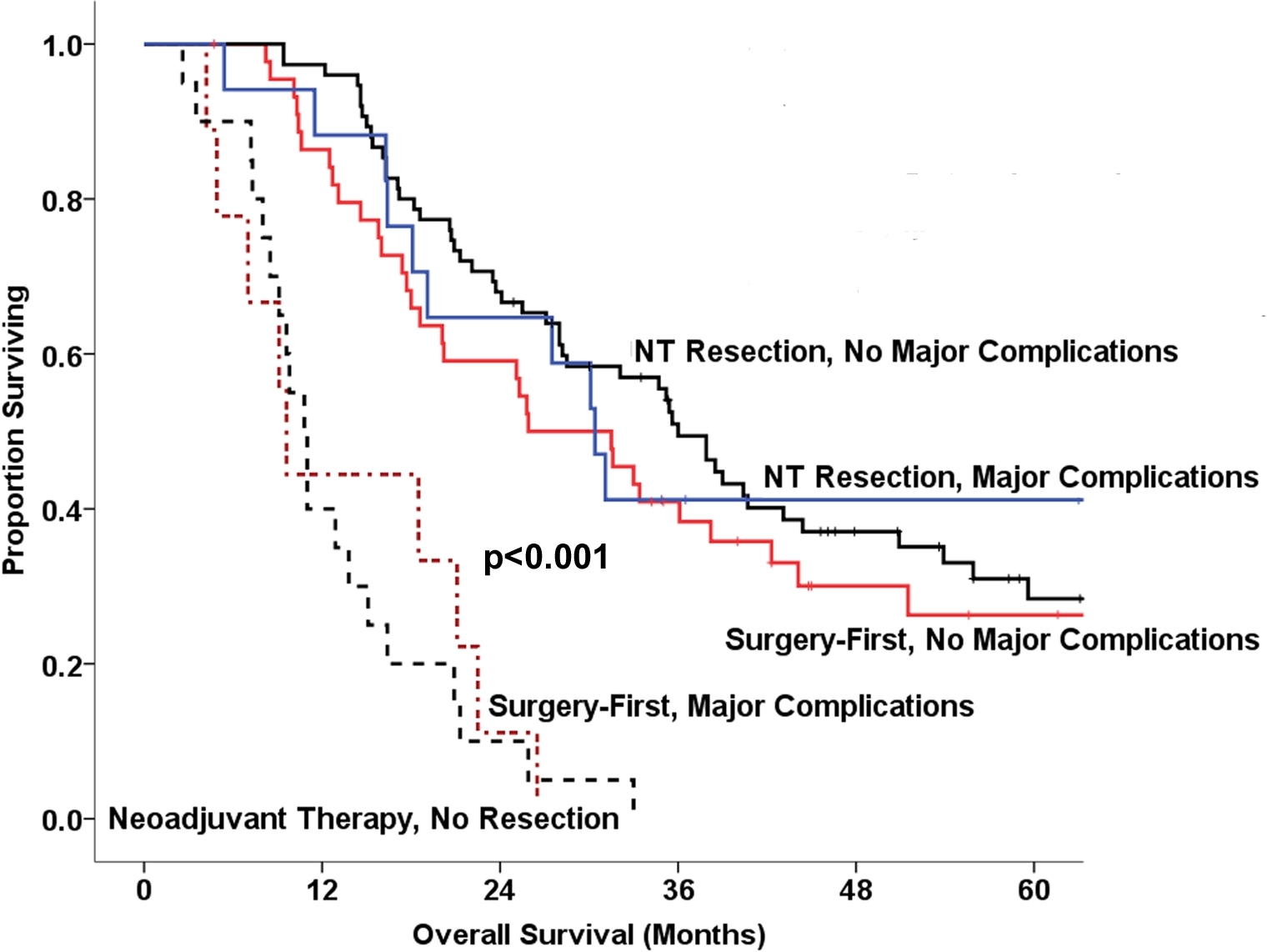
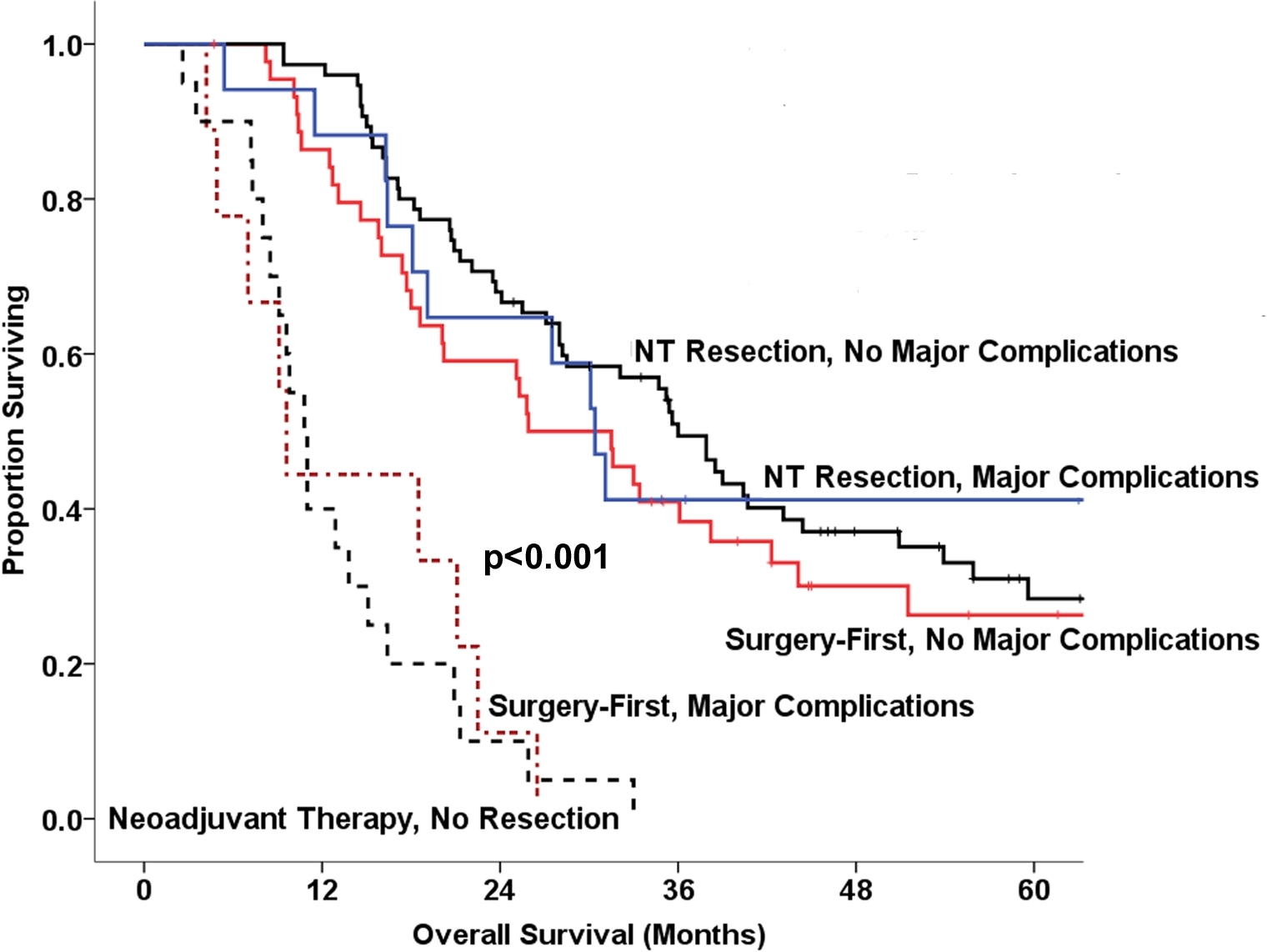
Among all patients, those who completed MMT lived longer than those who did not (36 vs. 11 mo, p<0.001). The median OS durations of all NT and SF patients (NT 28 vs. SF 21 mo, p=0.082), the subset in each cohort who completed MMT (NT 36 vs. SF 36 mo, p=0.565), and the subset in each cohort who did not complete MMT (NT 11 vs SF 13 mo, p=0.325) were not statistically different.
The rate of PMC did not differ between NT and SF groups (19% vs. 17%, p=0.782). SF patients with no PMC had a 71% (31/44) MMT completion rate vs. 25% (2/8) after PMC (p=0.014). When resected NT patients suffered PMC, there was no significant decrease in OS (36 vs. 30 mo, p=0.934), in contrast to the negative effect of PMC in SF patients (26 vs. 10 mo, p<0.001).
Conclusions: Completion of multimodality therapy is strongly associated with improved survival of operable patients with resectable PDAC. Even in the highly selected cohort evaluated in this study, early cancer progression and PMC negatively impacted MMT completion rates and OS, particularly among SF patients. Thus, NT sequencing remains a valuable alternative to SF sequencing for tumor biology evaluation and patient selection.
Back to Annual Meeting Program
|