|
Back to Annual Meeting Program
Predictors of Recurrence in Intraductal Papillary Mucinous Neoplasm: Experience With 208 Pancreatic Resections
Megan Winner*, Irene Epelboym, Joseph Dinorcia, Minna K. Lee, James a. Lee, Beth Schrope, John a. Chabot, John D. Allendorf
Department of Surgery, Columbia University College of Physicians and Surgeons, New York, NY
Background: Intraductal papillary mucinous neoplasm (IPMN) is being diagnosed and resected with increasing frequency, but little long-term data exist to guide postoperative management of surgically treated patients.
Methods: We examined all patients who underwent surgical resection for IPMN between January 1997 and April 2011 at our institution. IPMN was categorized as non-invasive low grade (adenoma and borderline dysplasia), non-invasive high grade (carcinoma in situ), or invasive. Histologic features of primary and recurrent disease were examined and we evaluated predictors of recurrence using Kaplan Meier curves and Cox proportional hazards models.
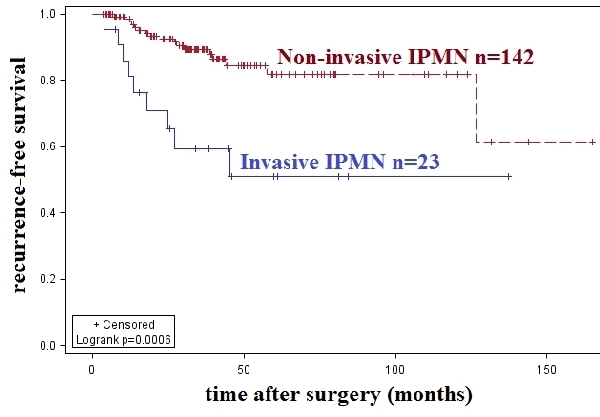
Results: Two hundred and eight patients underwent resection for IPMN. At presentation, 57% were symptomatic, 20% had a mural nodule or an associated mass, and median cyst size was 1.8cm. Sixty-eight (32.7%) operations for high grade disease were performed, of which 33 revealed invasive carcinoma. Among 165 R0 resections with greater than three months of follow-up we have observed 26 cases of recurrent disease over 502 person-years (median follow-up time 30.8 months). Nine (39%) patients originally diagnosed with invasive carcinoma and 17 (12%) patients originally diagnosed with non-invasive IPMN have recurred. Of the latter, four (23.5%) recurred as invasive carcinoma. Most disease recurred locally (25/26) but three individuals had concurrent metastatic disease at the first observation of recurrence. Median time from initial treatment to recurrence was 18.2 months, but ranged from 3.7 to 126.8 months. Invasive tumors were more likely to recur (HR 3.7, p=0.002) with a median time to recurrence of 13.5 months. Among non-invasive tumors, no single histologic feature—including dysplastic changes at the surgical margin or distant from the primary tumor—meaningfully predicted recurrence. Seven patients had a completion pancreatectomy on average 22.7 months after their initial surgery. Of these, three had low grade or moderate dysplasia on final pathology and have survived greater than 34 months after the second operation, compared with median survival of 14.4 months after diagnosis of recurrent, invasive IPMN.
Conclusions: Invasive IPMN has a high risk of recurrence, but even low grade tumors may recur with high grade disease. IPMN can recur remote from the time of primary surgery and no histologic feature beyond invasion predicts recurrence risk. Most recurrence is local and completion pancreatectomy can be associated with excellent survival if recurrent disease is identified early. We therefore recommend that surveillance of the remnant pancreas continue after primary resection for all tumor types.
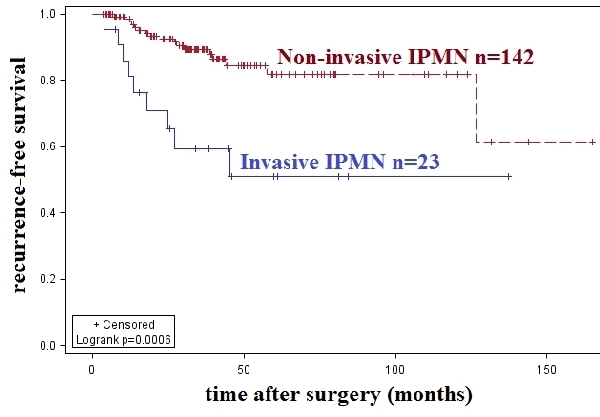
Recurrence-free survival among R0 resections for IPMN with at least three months follow up, stratified by invasive pathology. Non-invasive IPMN includes adenoma (76), borderline or moderate dysplasia (36), and carcinoma in situ(30). Median follow up was 30.8 months (502 person-years). Invasive IPMN was more likely to recur than non-invasive tumors (HR 3.7, 95% CI 1.7-8.4), with a median time to recurrence of 13.5 months. Of the 17 non-invasive IPMNs that recurred, four recurred with invasive disease.
Back to Annual Meeting Program
|