|
 |
Back to Annual Meeting Program
Pelvic Radiation Increases the Risk of Ileal Pouch Failure in Patients With Colorectal Cancer Complicating Inflammatory Bowel Disease
Xianrui Wu*1, Pokala R. Kiran1, Feza H. Remzi1, Saurabh Mukewar2, Bo Shen2
1Department of Colorectal Surgery, The Cleveland Clinic Foundation, Cleveland, OH; 2Department of Gastroenterology, The Cleveland Clinic Foundation, Cleveland, OH
Background:
The impact of preoperative radiation therapy on pouch function and survival has NOT been studied in ulcerative colitis (UC) patients with colorectal cancer (CRC) who undergo restorative proctocolectomy with ileal pouch-anal anastomosis (IPAA). The aim of this study was to evaluate pouch outcomes in UC-CRC-IPAA patients with or without preoperative radiation therapy.
Methods:
Patients with UC-CRC who underwent restorative proctocolectomy with IPAA from 1984-2009 were evaluated. Patients who underwent IPAA for medically refractory IBD or familial adenomatous polyposis, and patients whose initial pouch configuration was other than J or S type were excluded. Pouch failure was defined as the requirement of permanent diversion or pouch excision. The effect of pelvic radiation on pouch related outcomes was evaluated.
Results:
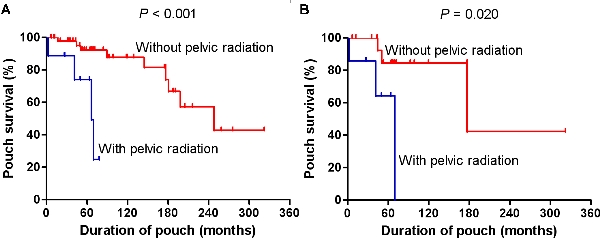
A total of 63 pouch patients with confirmed UC-CRC were included (37 male and 26 female). Mean age at pouch surgery was 46.9±10.6 years. Of the 63 patients, loop ileostomy was not closed in 2 patients, and 5 were lost to follow-up. Of the 56 patients eligible for final analysis, 9 patients received pelvic radiation. Among them, 5 patients had neo-adjuvant radiation, 2 received adjuvant radiation after colectomy but before IPAA, while 2 had prior radiation for previous cervical cancer. Pouch failure occurred in 13 patients after a median follow-up of 66.4 (range: 2.7-322.2) months, and 4 (30.8%) of them had radiation therapy. Causes of pouch failure included pouch/anal transition zone (ATZ) cancer (n=4), chronic pouchitis (n=3), pouch stricture (n=3), pelvic abscess (n=2), and incontinence (n=1). Pelvic radiation correlated significantly with chronic pouchitis (p=0.024). There was, however, no association between pelvic radiation and pouch/ATZ cancer, pouch stricture, pelvic abscess, and pouch fistula/sinus (p>0.05, Table). Kaplan-Meier analysis revealed that pelvic radiation was associated with poor pouch outcome (log-rank test, P<0.001, Figure). The impact of pelvic radiation on pouch outcome was further confirmed in the subgroup analysis of rectal cancer patients (log-rank test, P=0.020, Figure).
Conclusions:
Pelvic radiation even before IPAA creation is significantly associated with poor pouch outcomes in this small sample-sized, yet the largest study in the literature. This information needs to be considered and discussed with patients with prior RT undergoing IPAA. Further, the potential oncological benefits of chemo-radiation should be carefully balanced against any potential adverse effects on functional results on a case by case basis when deciding management of UC patients with CRC.
Demographic and clinicopathological characteristics
| Characteristic | All cases | Without pelvic radiation | With pelvic radiation | P value | | Number of patients | 63 | 52 | 11 | | | Histologic type, n (%) | | | | 0.69 | | Adenocarcinoma | 54 | 44 (84.6%) | 10 (90.9%) | | | Mucinous adenocarcinoma | 9 | 8 (15.4%) | 1 (9.1%) | | | Synchronous dysplasia, n (%) | 34 | 31 (59.6%) | 3 (27.3%) | 0.051 | | Histologic grade of tumor, n (%), | | | | 0.43 | | Poor | 20 | 16 (32.7%) | 4 (50.0%) | | | Well to moderate | 37 | 33 (67.3%) | 4 (50.0%) | | | Tumor location, n (%) | | | | 0.005 | | Rectum | 26 | 17 (32.7%) | 9 (81.8%) | | | Colon | 37 | 35 (67.3%) | 2 (18.2%) | | | TNM stage, n (%) | | | | 0.008 | | 0 + I + II | 35 | 33 (63.5%) | 2 (18.2%) | | | III + IV | 28 | 19 (36.5%) | 9 (81.8%) | | | Neo-adjuvant chemotherapy, n (%) | 6 | 0 (0.0%) | 6 (54.5%) | <0.001 | | Adjuvant chemotherapy, n (%) | 26 | 29 (36.5%) | 7 (63.6%) | 0.176 | | Configuration of pouch, n (%) | | | | 0.10 | | J pouch | 50 | 39 (75.0%) | 11 (100.0%) | | | S pouch | 13 | 13 (25.0%) | 0 (0.0%) | | | Method of anastomosis, n (%) | | | | 0.73 | | Stapled | 31 | 25 (51.0%) | 6 (60.0%) | | | Hand-sewn | 28 | 24 (49.0%) | 4 (40.0%) | | | Hospitalization, days | 8.1±3.5 | 8.0±3.6 | 8.1±2.8 | 0.95 | | Pelvic abscess, n (%) | 9 | 7 (14.9%) | 2 (22.2%) | 0.63 | | Pouch fistula/sinus, n (%) | 8 | 7 (14.9%) | 1 (11.1%) | 0.77 | | Pouch stricture, n (%) | 16 | 14 (29.8%) | 2 (22.2%) | 0.72 | | Chronic pouchitis, n (%) | 18 | 12 (25.5%) | 6 (66.7%) | 0.024 | | Pouch/ATZ neoplasia, n (%) | 7 | 6 (12.8%) | 1 (11.1%) | 0.89 |
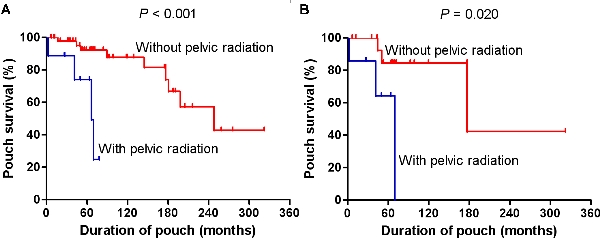
Impact of pelvic radiation on pouch outcome: Kaplan-Meier survival analysis with log-rank test. (A) All IBD-CRC patients, n=56; with pelvic radiation, n=9; without pelvic radiation, n=47. (B) IBD associated rectal cancer patients, n=24; with pelvic radiation, n=7; without pelvic radiation, n=17.
Back to Annual Meeting Program
|