|
Back to Annual Meeting Program
Staging and Survival of Resected Hilar Cholangiocarcinoma: an Analysis of 80 Consecutive Patients
Victor M. Zaydfudim*, Clancy J. Clark, Michael L. Kendrick, Florencia G. Que, Kaye M. Reid Lombardo, John H. Donohue, Michael B. Farnell, David M. Nagorney
Division of Gastroenterologic and General Surgery, Mayo Clinic, Rochester, MN
Introduction:
Predicting long-term survival in hilar cholangiocarcinoma is difficult. The revised AJCC staging system has not been extensively evaluated and may not correlate with clinical outcomes. An alternative staging system which incorporates factors related to local tumor extent, including portal vein invasion and lobar atrophy, has been proposed. The aim of this study was to evaluate current staging systems for hilar cholangiocarcinoma and identify clinical factors associated with improved survival.
Methods:
In this retrospective cohort study, clinical and pathologic characteristics were obtained for all resected patients with Bismuth-Corlette Type IIIa and IIIb hilar cholangiocarcinoma from 1993 to 2011. Patients were stratified by the 7th edition AJCC TNM staging parameters and by the modified Blumgart staging system which includes portal vein invasion and presence of lobar atrophy. Univariate and multivariate analyses were used to test effects of clinicopathologic factors and staging systems on overall survival.
Results:
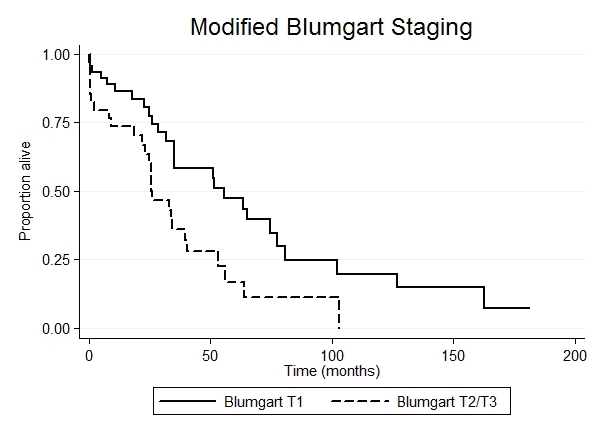
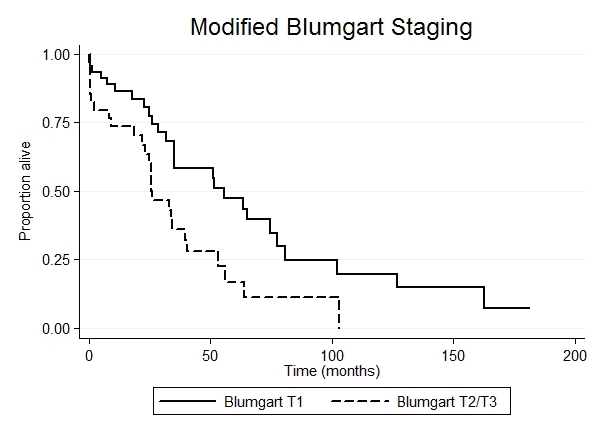
Eighty consecutive patients (median age 64 years (range 36-82), 64% male) underwent an anatomic hepatectomy with a bile duct resection and reconstruction for Bismuth-Corlette IIIa (51%) and Bismuth-Corlette IIIb (49%) cholangiocarcinoma. Margin negative resection was achieved in 94% of resections; 30-day mortality was 10%. Median follow-up was 26 months (range 0-181 months) with overall median survival of 34 months. Twenty-three percent of the patients had well-differentiated cholangiocarcinoma. The AJCC staging system stratified patients into following groups: T1-26%, T2-58%, T3-16%; N0-61%, N1-39%; Stage I-20%, Stage II-30%, Stage III-50%. None of the patients had distant metastases at the time of resection. Kaplan-Meier estimates did not demonstrate an association between survival and AJCC staging parameters (all p≥0.121). Blumgart staging system stratified patients into following groups: Blumgart T1 - 58%, Blumgart T2 - 41%; one patient had a Blumgart T3 cholangiocarcinoma with invasion into portal vein bifurcation. Univariate analyses demonstrated an association of survival with tumor grade (p=0.033) and Blumgart T-stage (p=0.010). One- and five-year survival estimates for Blumgart T1 and Blumgart T2/T3 were 86% and 47% vs. 74% and 17% (p=0.010). After adjusting for tumor grade, Blumgart T2/T3 stage correlated with increased likelihood of mortality (HR=1.93, 95%CI: 1.09-3.42, p=0.024)
Conclusions:
While the current AJCC TNM staging system did not predict survival in the current study, the Blumgart staging system which emphasizes portal vein invasion and lobar atrophy predicted overall survival independent of other clinical and pathologic factors. Inclusion of lobar atrophy into the T classification might improve accuracy of the AJCC system, and help define prognosis in patients with hilar cholangiocarcinoma.
Back to Annual Meeting Program
|