|
Back to Annual Meeting Program
Meta-Analysis of Trials Comparing Central and Distal Pancreatectomies : Short and Long-Term Outcomes
Mohammad Sarhan*1, Alan S. Rosman4, John D. Allendorf2, Leaque Ahmed1, Zahra Shafaee3
1Columbia University at Harlem Hospital Center, New York, NY; 2Columbia University College of physicians and surgeons, New York, NY; 3Lawrence Hospital, Bronxville, NY; 4Mount Sinai School of Medicine and Bronx VAMC, New York, NY
Introduction: Recent literature suggests superior pancreatic function after Central Pancreatectomy (CP) compared to Distal Pancreatectomy (DP) in patients with benign or low grade malignant neoplasms of the neck or body of pancreas. Available data is limited to single institutional studies with small sample size. In order to overcome these shortcomings, we performed the first systematic meta-analysis in this subject.
Methods: A systematic English literature review was performed using Pubmed database. All related articles comparing central and distal pancreatectomy from 1990 to 2010 were reviewed. The end-point was to compare peri-operative complication rate and long-term outcomes (new onset or worsening diabetes, tumor recurrence) after each procedure. Meta-analysis was performed based on random-effect model.
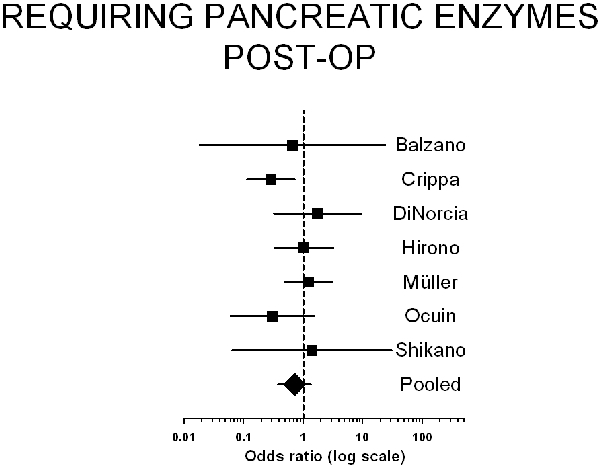
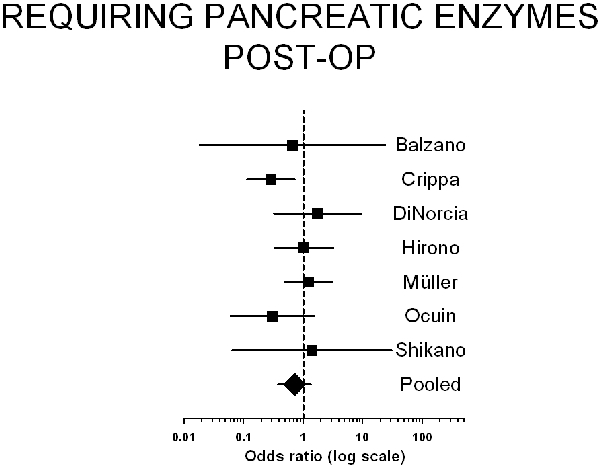
Results: Eight eligible studies were found, including 615 patients (CP: 343, DP: 272). Both groups were similar (age, sex, baseline pancreatitis, and incidence of IPMN and malignancy on final pathology). Baseline DM was higher in DP group (Odds Ratio: 0.35). Short term outcomes: CP was associated with longer Operative time (257 vs. 232min, P: 0.34) and less blood loss (378 vs. 651ml, P: 0.0006). Hospital stay was longer (12.75 vs. 9.63 days, P: 0.0038) and pancreatic fistula rate was higher in CP compared with DP (OR: 1.6, P: 0.04). Incidence of types B and C pancreatic fistulas were similar in two groups (OR: 1.3, P 0.44). The rate of new onset diabetes (OR: 0.11, P: 0.00) or worsening diabetes (OR: 0.03, P: 0.00) was significantly lower in the CP. There was no difference in tumor recurrence rate in both groups.
Conclusion: Our analysis suggests that CP is associated with lower rate of pancreaticogenic diabetes. This will justify for slight increase in operative time, pancreatic fistula rate, and length of hospital stay. Preservation of uninvolved pancreas leads to conservation of the pancreatic function and make CP a good alternative to more radical distal pancreatectomy for benign and low-grade malignant neoplasms.

Back to Annual Meeting Program
|