|
 |
Back to Annual Meeting Program
Foregut Surgery in the Modern Era: a National Survey
Zeling Chau*1, Jillian K. Smith1, Elan R. Witkowski1, Elizaveta Ragulin-Coyne1, Sing Chau NG1, Tara S. Kent3, Shimul a. Shah1, Jennifer F. Tseng2,1
1Surgical Outcomes Analysis & Research, University of Massachusetts Medical School, Worcester, MA; 2Division of Surgical Oncology, Beth Israel Deaconess Medical Center, Harvard Medical School, Boston, MA; 3Department of General Surgery, Beth Israel Deaconess Medical Center, Harvard Medical School, Boston, MA
Background: Foregut surgery is technically complex. In recent years, increasing attention has been paid to high-stakes surgery outcomes, including mortality and complications. In addition, the use of advanced technology including minimally invasive approaches has been introduced. The current study aims to determine national trends in utilization and outcomes of potentially curative cancer resections of the foregut, including esophagus, stomach, liver, and pancreas.
Methods: The Nationwide Inpatient Sample was queried to identify all esophageal, gastric, liver and pancreas resections performed for cancer during 1998-2009. Annual incidence, major in-hospital postoperative complications, length of stay and in-hospital mortality were evaluated. Univariate and multivariate analysis performed by chi square and logistic regression. For all comparisons, p-values <0.05 were considered statistically significant.
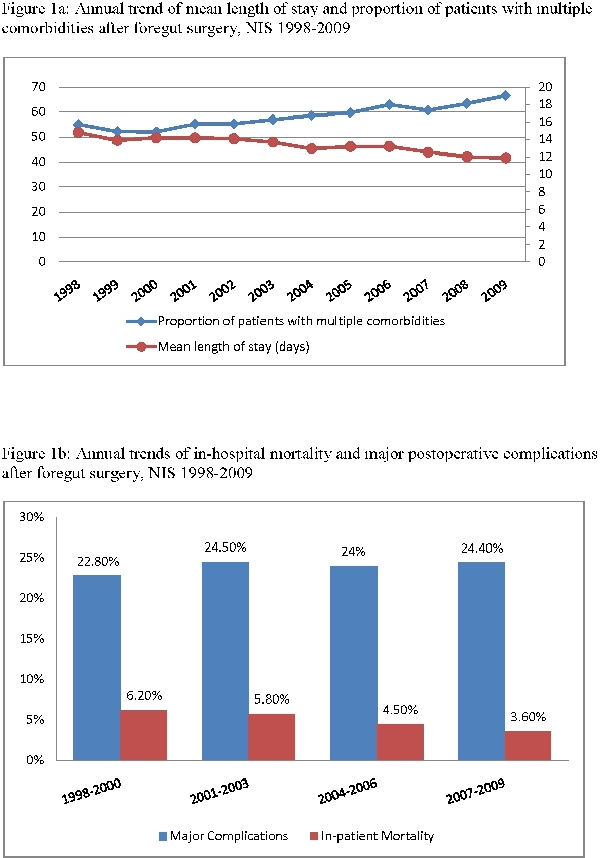
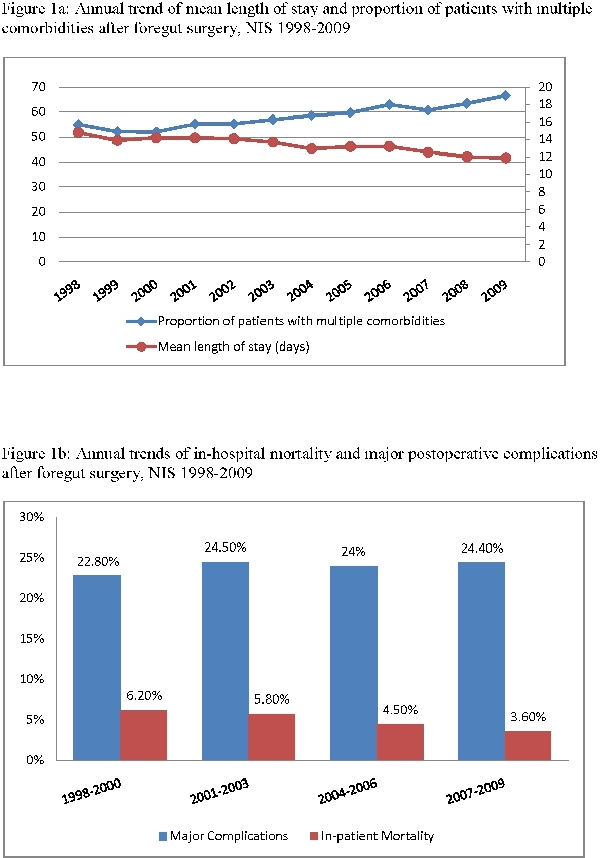
Results: 298,871 patients (nationally-weighted) underwent cancer directed foregut surgery 1998-2009. Of those 19,002 (6%) were esophagectomies, 123,198 (41%) were gastrectomies, 62,313 (21%) were hepatectomies and 94,358 (32%) were pancreatectomies. From early years (1998-2000) to late years (2007-2009) use of laparoscopy in foregut surgery increased from 3% to 5%. Laparoscopy in esophagectomy increased the most from 1% to 5%, while its use in hepatectomy remained unchanged at 4%. Gastrectomy and pancreatectomy involving minimally invasive techniques increased from 2% to 5% and 5% to 6%, respectively. For all four foregut surgery types, patient comorbidities increased over time; patients with ≥2 major comorbidities increased from 53% to 64%. Conversely, patient mortality and length of stay (LOS) decreased over time. However, we observed an increase in complications for all sites combined from 22.8% to 24.4%. Laparoscopy was not significantly associated with decreased complications, but was associated with lower mortality when compared to open resection alone 3.1% vs. 5%. Independent predictors of increased complications included older age, gender, higher comorbidity, hospital volume. Older age, male sex, higher comorbidity, low volume center and non-use of laparoscopy were independent predictors of in-hospital mortality.
Conclusion: Foregut surgery in the modern era is being increasingly deployed on sicker patients. While decreased in-hospital mortality and LOS are commendable, complication rates remain substantial and nondecreasing. Minimally invasive techniques have minor but increasing penetrance in foregut surgery. Our results suggest comparable advances and potential pitfalls among major types of foregut surgery in the current era.
Back to Annual Meeting Program
|